Abstract
Diabetes is one of the most common chronic diseases, so that the number of diabetics was 221 million worldwide in 2010. Diabetes has no decisive cure and can lead to fatal complications. This disease is the most common cause of amputation, blindness and chronic renal failure and one of the most important risk factors for coronary heart diseases (Masoudi et al., 2004). The global incidence of diabetes is increasing due to the increased obesity and decreased physical activity (Bidarpour et al., 2003). Non-insulin dependent or type 2 diabetes is now an epidemic in the United States; and it had the prevalence of 7 percent in adults over 30 years in 2000 (Hillier and Pedula, 2001).
Letter to Editor
Diabetes is one of the most common chronic diseases, so that the number of diabetics was 221 million worldwide in 2010. Diabetes has no decisive cure and can lead to fatal complications. This disease is the most common cause of amputation, blindness and chronic renal failure and one of the most important risk factors for coronary heart diseases Masoudi et al., 2004. The global incidence of diabetes is increasing due to the increased obesity and decreased physical activity Bidarpour et al., 2003. Non-insulin dependent or type 2 diabetes is now an epidemic in the United States; and it had the prevalence of 7 percent in adults over 30 years in 2000 Hillier and Pedula, 2001.
Despite the fact that the complete prevention of diabetes complications is not possible, the evidence suggests that the Glycemic control in diabetic patients can delay or reduce the incidence of debilitating and even fatal diabetes complications Pringle et al., 1993.
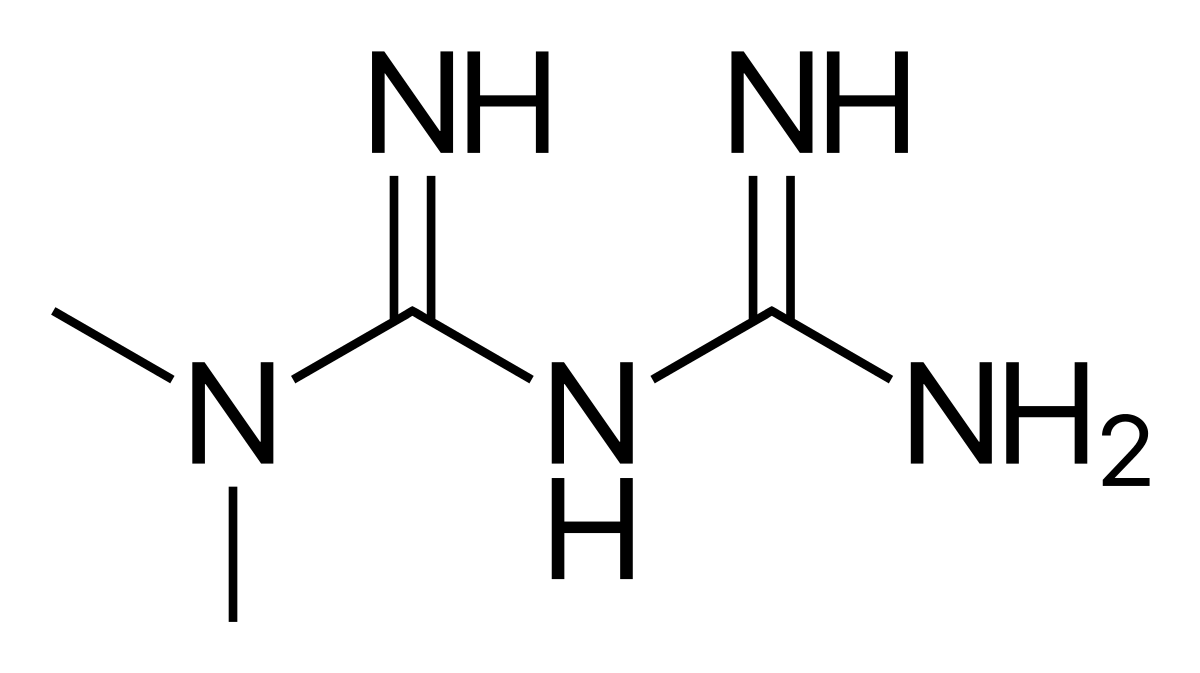
Based on the recommendations of the American Diabetes Association, the treatment should be started by changes in lifestyle and taking Metformin in diabetic patients with proper renal function with the aim at achieving the level of glycosylated hemoglobin (HbA1c) equal to or less than 7% Fenton et al., 2006. Typically, the patients should take another supplemental drug in addition to Metformin in order to achieve this goal. However, there is not any scientific evidence or consensus on the type of received medication by patient as the adjunct therapy Inzucchi et al., 2012.
Clinicians utilize insulin for fast and flexible control of blood glucose levels. Furthermore, several studies of clinical trial have found that the early start of insulin is effective in preserving the beta cell function Harrison et al., 2012. Accordingly, the insulin therapy is increasingly associated with monotherapy of Metformin as the adjunctive therapy Holden et al., 2011. However, most of the patients tend to postpone the use of insulin because of concern about difficult insulin injection, hypoglycemia and overweight. According to study by Roumie et al, the risk of diabetes complications and mortality is higher in group of patients, who receive insulin plus Metformin, compared to a group of patients who receive Metformin and Sulfonylureas, so that the ratio of adjusted risk is equal to 1.21 (1.07-1.58, 95% CI) for cardiovascular disease and overall mortality, and 1.44 (1.15-1.79, 95% CI) for all-cause mortality, 1.21 (0.74-2, 95% CI) for death from cardiovascular disease, and 1.85 (1.21-2.84, 95% CI) for death from cancer. Therefore, due to the insufficient scientific evidence, it is difficult to make decisions about the use of insulin or Sulfonylureas as the adjunct therapy to Metformin Roumie et al., 2014. Therefore, it is suggested conducting more clinical and epidemiological trials for determining the best drug as the intensified therapy in diabetic patients, so that the clinicians can more effectively select and prescribe the best drug combination for treatment of diabetics based on the obtained results.
Abbreviations
CI: Confidence Interval
HbA1c: glycated haemoglobin (A1c)
References
-
F.
Bidarpour,
N.K.
HOLAKOUEI,
A.
Rahimi,
N.
ESMAEILNASAB.
A survey of risk factors for type 2 diabetes in patients of Kurdistan Diabetic Center in 2001. Scientific Journal of Kurdistan university of medical sciences.
2003;
:
20-35
.
-
J.J.
Fenton,
M.
Von Korff,
E.H.
Lin,
P.
Ciechanowski,
B.A.
Young.
Quality of preventive care for diabetes: effects of visit frequency and competing demands. The Annals of Family Medicine.
2006;
4
:
32-39
.
-
L.B.
Harrison,
B.
Adams -Huet,
P.
Raskin,
I.
Lingvay.
beta-cell function preservation after 3.5 years of intensive diabetes therapy. Diabetes Care.
2012;
35
:
1406-1412
.
-
T.A.
Hillier,
K.L.
Pedula.
Characteristics of an adult population with newly diagnosed type 2 diabetes. Diabetes care.
2001;
24
:
1522-1527
.
-
S.E.
Holden,
C.D.
Poole,
C.L.
Morgan,
C.J.
Currie.
Evaluation of the incremental cost to the National Health Service of prescribing analogue insulin. BMJ open.
2011;
1
:
e000258
.
-
S.E.
Inzucchi,
R.M.
Bergenstal,
J.B.
Buse,
M.
Diamant,
E.
Ferrannini,
M.
Nauck,
A.L.
Peters,
A.
Tsapas,
R.
Wender,
D.R.
Matthews.
Management of hyperglycemia in type 2 diabetes: a patient -centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care.
2012;
35
:
1364-1379
.
-
A.N.
Masoudi,
F.
Ghofranipour,
F.
Ahmadi,
G.H.
Babaei,
A.
Rajab.
Evaluation of effectiveness of community based interventions on controlling diabetes mellitus in Tehran, 1382. Iranian Journal of Diabetes And Lipid Disorders.
2004;
:
85-93
.
-
M.
Pringle,
C.
Stewart-Evans,
C.
Coupland,
I.
Williams,
S.
Allison,
J.
Sterland.
Influences on control in diabetes mellitus: patient, doctor, practice, or delivery of care?. Bmj.
1993;
306
:
630-634
.
-
C.L.
Roumie,
R.A.
Greevy,
C.G.
Grijalva,
A.M.
Hung,
X.
Liu,
H.J.
Murff,
T.A.
Elasy,
M.R.
Griffin.
Association between intensification of metformin treatment with insulin vs sulfonylureas and cardiovascular events and all-cause mortality among patients with diabetes. Jama.
2014;
311
:
2288-2296
.
Comments
Downloads
Article Details
Volume & Issue : Vol 4 No 06 (2017)
Page No.: 1341-1343
Published on: 2017-06-24
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 3711 times
- Download PDF downloaded - 1252 times
- View Article downloaded - 18 times
 Biomedpress
Biomedpress

