Abstract
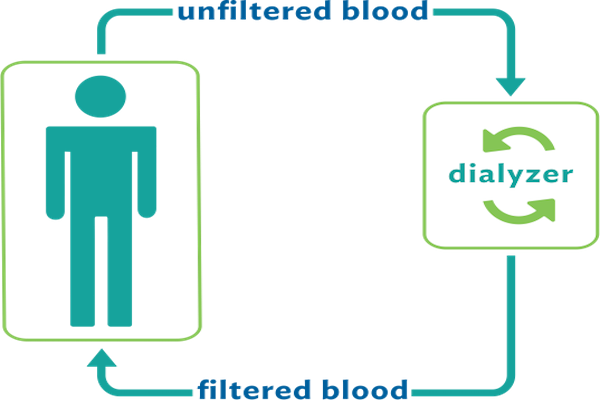
Chronic kidney disease (CKD) is known as a major health problem worldwide (Levey et al., 2007). The CKD is defined as a stage of disease in which the patient's kidney function is less than a half of normal capacity (2). If the kidney function is 10% to 15% less than the normal capacity, the patient has reached the End Stage Renal Disease (ESRD). At this stage, the kidney transplant or dialysis with hemodialysis or peritoneal dialysis is necessary for patient's survival (Levey et al., 2002).
Letter
The incidence of ESRD is rapidly increasing globally, so that the incidence of disease has had the ten-time increased in America during the past few years Health and Services, 2011. On average, the number of patients, who receive hemodialysis treatment, has had the annual increase of approximately 7% Lysaght, 2002. The prevalence of this disease varies in different parts of world. The highest incidence belongs to Taiwan with 2447 patients per one million people, but the lowest incidence belongs to the Philippines with 110 patients per one million people Mongoh et al., 2008.
There is a significant statistical relationship between the anemia with low survival in patients with chronic renal failure undergoing the hemodialysis Pfeffer et al., 2009Singh et al., 2006. In recent years, the Erythropoiesis-stimulating agent (ESA) has been widely used as a treatment for anemia in patients with chronic kidney disease (CKD) and patients with ESRD. However, the treatment of anemia results in the increased survival rates in these patients. According to the conducted clinical trial studies, the modified hemoglobin (Hb) rate to normal range through Erythropoiesis-stimulating agent (ESAs) will not lead to the improved outcomes in these patients Besarab et al., 1998Drüeke et al., 2006Pfeffer et al., 2009Singh et al., 2006, so that the ratio of myocardial infarction, congestive heart failure, stroke, hospitalization and mortality in a group with target hemoglobin level of 13g/dL is higher than the target hemoglobin level of 11g/dL in a randomized clinical trials Pfeffer et al., 2009. Therefore, the higher dose of Erythropoietin in patients with higher target hemoglobin level leads to an increased risk of death and non-improved life quality compared to the group with lower target levels.
According to a research by Elani Streja et al for investigating the relationship between the received dose of Erythropoietin and mortality in dialysis patients, there is a positive dose-response relationship between weekly dose of Erythropoietin drug and the risk of death. According to this study, the higher dose of Erythropoietin drug is along with increased mortality, so that compared to base group (group with weakly does of less than 6000 units), the ratio of mortality in patients with weekly doses of 6000 to less than 12,000 units is equal to (1.02 95% CI 0.94-1.1), and (1.08 95% CI 1-1.18) in group with a weekly dose of 12,000 to less than 18,000 units, and (1.17 95% CI 1.06-1.28) in group with a weekly dose of 18,000 to less than 24,000 units, and (1.27 95% CI 1.15-1.41) in group with a weekly dose of 24,000 to less than 30,000 units, and finally (1.52 95% CI 1.37 to 1.69) in group with a weekly dose of 30,000 units and higher Streja et al., 2016. Therefore, the scientific guidelines are approved and it is suggested modifying the partial hemoglobin levels in dialysis patients by erythropoietin drug, but it is not recommended obtaining the same hemoglobin level as the healthy people's standard levels in these patients by Erythropoietin drug Drüeke et al., 2006.
Abbreviations
CKD:Chronic kidney disease
CI:Confidence Interval
ESAs: Erythropoiesis-stimulating agent
ESRD: End Stage Renal Disease
References
-
A.
Besarab,
W.K.
Bolton,
J.K.
Browne,
J.C.
Egrie,
A.R.
Nissenson,
D.M.
Okamoto,
S.J.
Schwab,
D.A.
Goodkin.
The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. New England Journal of Medicine.
1998;
339
:
584-590
.
-
T.B.
Drüeke,
F.
Locatelli,
N.
Clyne,
K.-U.
Eckardt,
I.C.
Macdougall,
D.
Tsakiris,
H.-U.
Burger,
A.
Scherhag.
Normalization of hemoglobin level in patients with chronic kidney disease and anemia. New England Journal of Medicine.
2006;
355
:
2071-2084
.
-
U.D.o.
Health,
H.
Services.
Kidney disease statistics for the United States. Bethesda, MD: National Kidney and Urologic Diseases Information Clearinghouse, National Institutes of Health.
2011
.
-
A.
Levey,
R.
Atkins,
J.
Coresh,
E.
Cohen,
A.
Collins,
K.-U.
Eckardt,
M.
Nahas,
B.
Jaber,
M.
Jadoul,
A.
Levin.
Chronic kidney disease as a global public health problem: approaches and initiatives-a position statement from Kidney Disease Improving Global Outcomes. Kidney international.
2007;
72
:
247-259
.
-
A.S.
Levey,
J.
Coresh,
K.
Bolton,
B.
Culleton,
K.S.
Harvey,
T.A.
Ikizler,
C.A.
Johnson,
A.
Kausz,
P.L.
Kimmel,
J.
Kusek.
K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. American Journal of Kidney Diseases.
2002;
39
.
-
M.J.
Lysaght.
Maintenance dialysis population dynamics: current trends and long-term implications. Journal of the American Society of Nephrology.
2002;
13
:
S37-S40
.
-
M.N.
Mongoh,
N.W.
Dyer,
C.L.
Stoltenow,
M.L.
Khaitsa.
Risk factors associated with anthrax outbreak in animals in North Dakota, 2005: a retrospective case-control study. Public Health Reports.
2008;
123
:
352-359
.
-
M.A.
Pfeffer,
E.A.
Burdmann,
C.-Y.
Chen,
M.E.
Cooper,
D.
de Zeeuw,
K.-U.
Eckardt,
J.M.
Feyzi,
P.
Ivanovich,
R.
Kewalramani,
A.S.
Levey.
A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. New England Journal of Medicine.
2009;
361
:
2019-2032
.
-
A.K.
Singh,
L.
Szczech,
K.L.
Tang,
H.
Barnhart,
S.
Sapp,
M.
Wolfson,
D.
Reddan.
Correction of anemia with epoetin alfa in chronic kidney disease. New England Journal of Medicine.
2006;
355
:
2085-2098
.
-
E.
Streja,
J.
Park,
T.-Y.
Chan,
J.
Lee,
M.
Soohoo,
C.M.
Rhee,
O.A.
Arah,
K.
Kalantar-Zadeh.
Erythropoietin dose and mortality in hemodialysis patients: marginal structural model to examine causality. International journal of nephrology 2016.
2016
.
Comments
Downloads
Article Details
Volume & Issue : Vol 4 No 07 (2017)
Page No.: 1432-1434
Published on: 2017-07-28
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 5024 times
- Download PDF downloaded - 1434 times
- View Article downloaded - 9 times
 Biomedpress
Biomedpress

