Abstract
Introduction: Understanding the epidemiology of Esophageal Cancer (EC) seems to be essential in order to plan and control it. The aim of this study was to investigate the incidence and mortality rate of EC and its relationship with the worldwide Human Development Index (HDI) of 2012.
Methods: This study was an ecological study which assessed the correlation of age-standardized incidence rate (ASIR) and age-standardized mortality rate (ASMR) of EC with HDI and its components. ASIR and ASMR data for EC were extracted from the global cancer project for the year 2012. Statistical analyses were performed by SPSS 16.
Results: From EC were recorded worldwide in 2012, there was a total of 455,784 incidents of EC (70.86% males and 29.14% females; ratio of males to females was 2.43:1) and 400,169 mortalities (70.27% males and 29.73% females; ratio of males to females was 2.36:1). The correlation between HDI and SIR was -0.121 (p=0.105); with -0.061 (p=0.415) for men and -0.190 (p=0.010) for women. Moreover, the correlation between HDI and SMR was -0.156 (p=0.036), with -0.101 (p=0.180) for men and -0.218 (p=0.003) for women.
Conclusion: The incidence and mortality rates from EC is higher in less developed or developing countries. No statistically significant correlation was seen between the standardized mortality or incidence rates of EC and the 2012 HDI.
Introduction
Esophageal Cancer (EC) is the eighth most common cancer in terms of incidence and the sixth highest in terms of mortality Pennathur et al., 2013. In 2013, 442,000 new cases and 440,000 deaths were reported Ferlay et al., 2015. EC has caused 8.9 million daily worldwide in 2013; moreover, EC cancer has reached the 6th highest in terms of mortality (it ranked 7th for years of life lost (YLL) in 1990) Di Pardo et al., 2016. Eighty-four of EC have occurred in developing countries and 16% have occurred in developed ones Umar and Fleischer, 2008. Despite medical developments in recent years, the 5-year survival rate of EC has been <20% Castro et al., 2014Napier et al., 2014. The age-standardized incidence rate (ASIR) and age-standardized mortality rate (ASMR) per hundred thousand for esophagus cancer in both sexes from 2013 were greater in developing countries than in developed ones (ASIR=8.94 vs. 3.90, and ASDR=9.11 vs. 3.79, respectively) Ferlay J, 2013.
The highest rates of EC in men were seen in Eastern Asia (ASDR=22.4; ASIR=22.04) and in women were seen in the region of Eastern Sub-Sahara of Africa (ASDR=13.78; ASIR=12.74). The lowest rates for both sexes were seen in the region of Latin America (ASMR=2.49 and ASIR=2.14 for men; ASMR=0.64 and ASIR=0.64 for women) Ferlay J, 2013. Thus, EC occurs more frequently in men than women. In Iran, for instance, the frequency in men versus women is 2 to 4 times greater Kiadaliri, 2014. The highest incidence rate of EC has been observed in northern Iran, China, and southern Africa Castro et al., 2014Kiadaliri, 2014. Cancer incidence rates in these areas have been reported to be higher than 100 per hundred thousand Chen et al., 2015Harirchi et al., 2014. The greatest SIR of EC was seen in Malawi (as was the greatest SMR) and the greatest MIR was seen in China Torre et al., 2015.
Squamous cell carcinoma (SCC) and adenocarcinoma (ADC) are the two main histological types of EC Umar and Fleischer, 2008. The etiology and risk factors of these two types are different Spechler, 2013. Most cases of EC are of the SCC type Zhang, 2013. For unknown reasons, the incidence of SCC has declined in recent years while the incidence of ADC has increased Kim et al., 2014. EC is one of the cancers that are strongly associated with social and economic status Dar et al., 2013Wang et al., 2015. Studies have shown that tobacco, weak nutrition and alcohol are most associated with EC, especially the SCC type Lin et al., 2013Liu et al., 2014Salehi et al., 2013. Furthermore, low income populations have a higher chance of mortality from EC because they have less access to prevention and treatment services Wang et al., 2013Wei et al., 2015.
The Human Development Index (HDI) is a tool used to differentiate countries based on three components: life expectancy at birth, mean years of schooling, and income levels. The numerical value of the HDI is between 0 to 1 Malik, 2013a. Few studies have paid attention to the role and correlation of HDI and some types of cancer Ghoncheh et al., 2015aGhoncheh et al., 2015bHassanipour-Azgomi et al., 2016. Due to the high incidence of EC worldwide and the relevance of the HDI for understanding incidence and mortality related to EC, this study herein was undertaken to explore the relationship of the incidence and mortality of EC around the world with the 2012 HDI.
Materials - Methods
This study was an ecological study of global data to assess the correlation of ASIR and ASMR of EC with HDI 2012 and its components (including life expectancy at birth, mean years of schooling, and gross national income (GNI) per capita). Data on ASIR and ASMR for every country in 2012 were obtained from the global cancer project, available at http://globocan.iarc.fr/Default.aspx Ferlay et al., 2015, and from the HDI of the Human Development Report 2013 Malik, 2013b, which includes information from the 2012 HDI and corresponding details for each country in the world.
Method to estimate ASIR and ASMR from the global cancer project by international research agencies have previously been reported Ferlay et al., 2015Razi et al., 2016. HDI was obtained from a composite measure of indicators of three main components (including life expectancy, educational attainment, and command over resources needed for a decent living) Malik, 2013a.
Statistical analysis
In this study, we used correlation bivariate method to assess the correlation between ASR and HDI (and its corresponding components). Statistical significance was assumed if p<0.05. All reported p-values were two-sided. Statistical analyses were performed using SPSS (Version 16.0, SPSS Inc., Chicago, IL).
Results
Overall, in 2012, 455,784 cases of EC were recorded around the world, of which 323,008 cases (70.86%) occurred in men and 132,776 cases (29.14%) occurred in women. The ratio, therefore, for men versus women was 2.43. The five countries with the largest number of new cases were as follows:
1) China (with about 223,306 cases),
2) India (with 41,774 cases),
3) Japan (with 19,683 cases),
4) United States of America (with 16,968 cases),
5) Bangladesh (with 13,909 cases).
Altogether, these 5 countries accounted for 315,640 cases (69.25%) of all incidents of EC worldwide.
As for highest SIR of EC in the world, the top five countries were as follows:
1) Malawi (with SIR of 24.2 per hundred thousand people),
2) Turkmenistan (with 19.7 per hundred thousand people),
3) Kenya (with 17.6 per hundred thousand people),
4) Mongolia (with 17.6 per hundred thousand people),
5) Uganda (with 17.1 per hundred thousand people).
Furthermore, as for lowest SIR of EC, the top 5 countries were:
1) Vanuatu (with 0 per hundred thousand people),
2) Cape Verde (with 0.1 per hundred thousand people),
3) Solomon Islands (with 0.2 per hundred thousand people),
4) Western Sahara (with 0.2 per hundred thousand people),
5) Nigeria (with SIR of 0.3 per hundred thousand people).
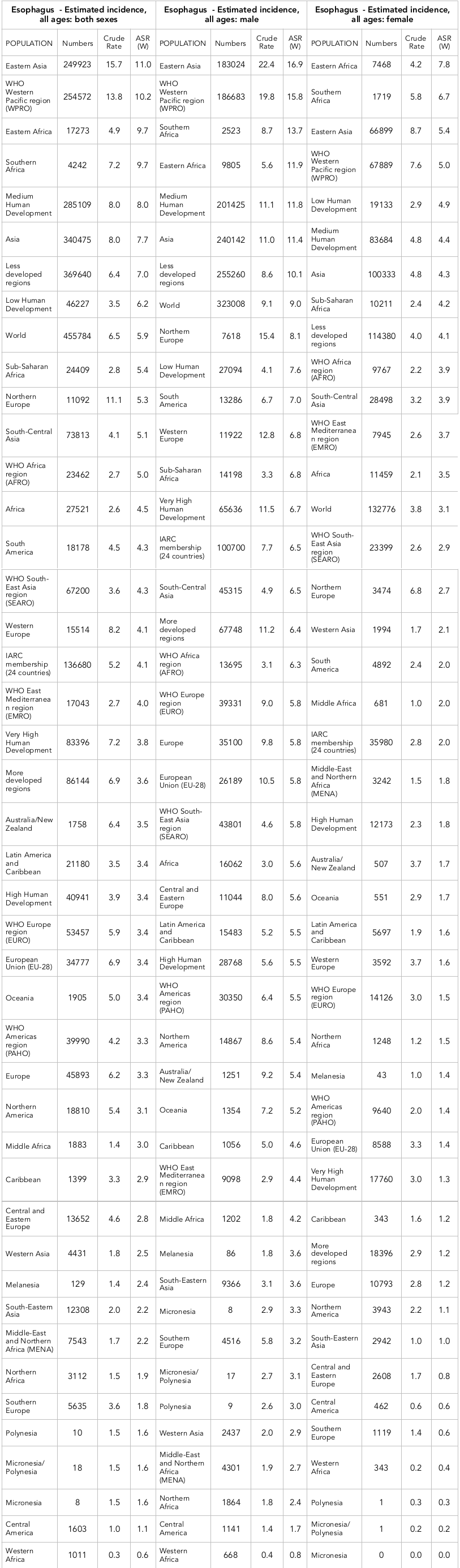
Based on the HDI, the SIR was 3.8% per hundred thousand people in Very High Human Development areas, 3.4% per hundred thousand people in High Human Development regions, 8 per hundred thousand people in Medium Human Development areas, and 6.2 per hundred thousand people in Low Human Development regions. Moreover, the SIR in the six WHO areas were: 3.4 per hundred thousand people in WHO Europe region (EURO), 3.3 per hundred thousand people in WHO Americas region (PAHO), 10.2 per hundred thousand people in WHO Western Pacific region (WPRO), 4.3 per hundred thousand people in WHO South-East Asia region (SEARO), 4 per hundred thousand people in WHO East Mediterranean region (EMRO), and 5 per hundred thousand people in WHO Africa region (AFRO). Additionally, there were 3.6 per hundred thousand people in more developed regions and 7 per hundred thousand people in less developed regions.
The number and rate of crude and SIR of EC worldwide in 2012 are shown in Table 1 according to regions in the world. Different regions of the world have been sorted from highest to lowest on the basis of SIR ( Table 1 ). Moreover, regions with the highest and lowest standardized rates of EC are depicted for each sex ( Table 1 ).
In terms of mortality, 400,169 cases of death have occurred worldwide in 2012 due to EC, of which 281,217 cases (70.27%) occurred in men and 118,952 cases (29.73%) occurred in women. Therefore, the ratio in men versus women was 2.36. The greatest number of deaths from EC occurred in these 5 countries:
1) China (with 197,472 cases),
2) India (with 38,683 cases,
3) United States of America (with 15,982 cases),
4) Bangladesh (with 12,909 cases),
5) Japan (with 12440 cases).
Altogether, these 5 countries accounted for 277,486 cases (69.34%) of all deaths from EC worldwide.
As for highest SMR of EC in the world, the top five countries were as follows:
1) Malawi (with standardized rate of 22.9 per hundred thousand people),
2) Turkmenistan (with 18.5 per hundred thousand people),
3) Kenya (with 16.5 per hundred thousand people),
4) Uganda (with 15.9 per hundred thousand people),
5) Mongolia (with 15.5 per hundred thousand people).
Furthermore, as for lowest SMR of EC, the top 5 countries were:
1) Vanuatu (with standardized rate of 0 per hundred thousand people),
2) Cape Verde (with 0.1 per hundred thousand people),
3) Solomon Islands (with 0.2 per hundred thousand people),
4) Western Sahara (with 0.2 per hundred thousand people),
5) Nigeria (with 0.3 per hundred thousand people)
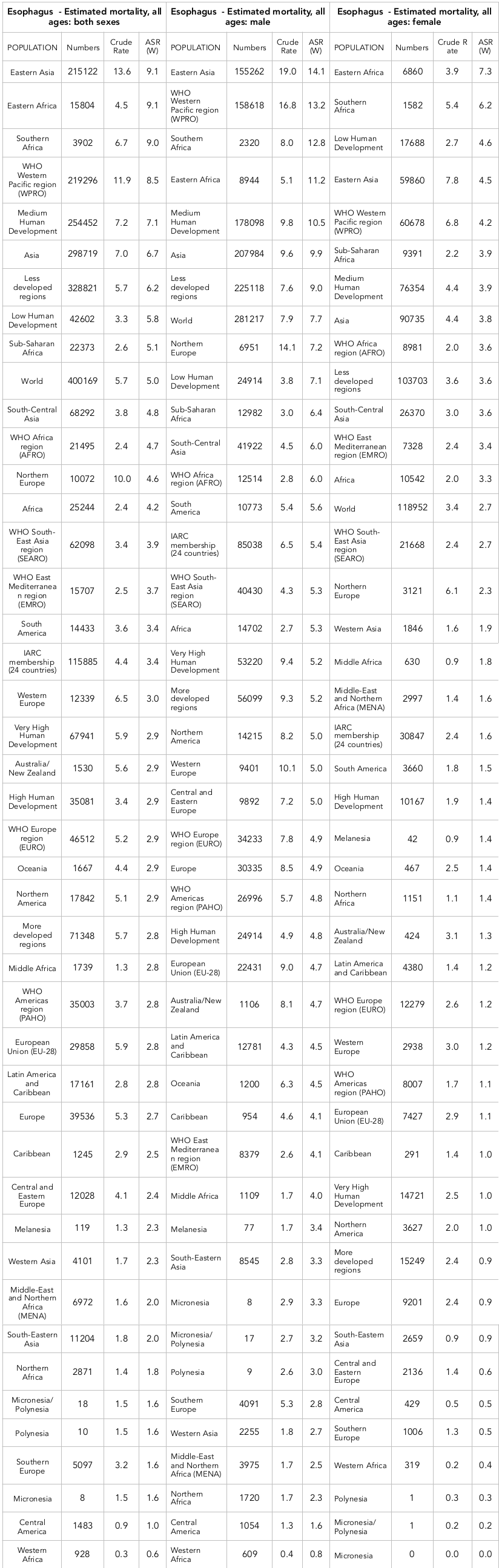
Human Development areas, 2.9 per hundred thousand people in High Human Development areas, 7.1 per hundred thousand people in Medium Human Development areas, and 5.8 per hundred thousand people in Low Human Development areas. Moreover, the SIR in the six WHO areas were 2.9 per hundred thousand people in WHO Europe region (EURO), 2.8 per hundred thousand people in WHO Americas region (PAHO), 8.5 per hundred thousand people in WHO Western Pacific region (WPRO), 3.9 per hundred thousand people in WHO South-East Asia region (SEARO), 3.7 per hundred thousand people in WHO East Mediterranean region (EMRO), and 4.7 per hundred thousand people in WHO Africa region (AFRO). Additionally, there were 2.8 per hundred thousand people in more developed regions and 6.2 per hundred thousand people in less developed regions.
The number and rate of crude and SMR of EC worldwide in 2012 are shown in Table 2 . Different parts of the world were sorted by standardized rates from high to low. The various parts of the world with the highest and lowest standardized rates of EC are depicted for each sex ( Table 2 ).
Correlation of SIR and HDI
A negative correlation (r=-0.121) was observed between SIR of EC and HDI; however, this correlation was not statistically significant (p=0.105). As well, there was a nonsignificant correlation between the components of the HDI and SIR for EC. For instance, between SIR and life expectancy at birth, there was a negative correlation (-0.124; p=0.099), between SIR and mean years of education the correlation coefficient was -0.054 (p=0.471), and between SIR and income level per capita the correlation coefficient was -0.024 (p=0.750). However, none of the above correlations were significant.
In men, a negative correlation (-0.061) was observed between SIR of EC and HDI, which was not statistically significant (p=0.415). A negative correlation (-0.092) was seen between SIR and life expectancy at birth (p=0.220), no correlation was seen between SIR and mean years of education, and a negative correlation (-0.025) was seen between SIR and income level per capita (p=0.744). However, none of the above correlations were significant.
In women, a negative correlation (-0.190) was observed between SIR of EC and HDI, which was not statistically significant (p=0.415). A negative correlation (-0.157) was seen between SIR of EC and life expectancy at birth (p=0.036), which was significantly significant. However, there was a negative correlation (-0.117) with mean years of education (p=0.119), and with income level per capita (-0.73; p=0.333), though neither was statistically significant.
Correlation of SMR and HDI
A negative correlation (-0.156) was observed between SMR of EC and HDI; this association was statistically significant (p=0.036). Also, a negative correlation (-0.154) was seen between SMR and life expectancy at birth (p=0.039), between SMR and mean years of education (-0.083; p=0.267), and between SMR and income level per capita (-0.051; p=0.499).
In men, a negative correlation (-0.1) was observed between SMR of EC and HDI though the association was not statistically significant (p=0.180). Specifically, a negative correlation (-0.126) was seen between SMR and life expectancy at birth (p=0.092), between SMR and mean years of education (-0.033; p=0.656), and between SMR and income level per capita (-0.008; p=0.910).
In women, a negative correlation (-0.218) was observed between SMR of EC and HDI, which was statistically significant (p=0.003). Also, a negative correlation (-0.180) was seen between the SMR and life expectancy at birth (p=0.015), between SMR and mean years of education (-0.139; p=0.063), and between SMR and income level per capita (-0.090; p=0.227).
Discussion
The results of our study showed that a negative relationship exists between the standardized incidence of EC and HDI, but that this relationship is not statistically significant. The statistics show that the highest incidence of EC were seen in Malawi, Turkmenistan and Kenya, respectively, in 2012. These findings were similar to other studies of Asian countries Pakzad et al., 2016. For instance, countries such as Turkmenistan, Mongolia, Tajikistan and China were shown to have the highest incidence of EC and are located in the Asian Esophageal Cancer Belt Ferlay et al., 2015Lin et al., 2013. These countries and some African countries which have high incidence of EC are all among the countries with average or poor HDI Malik, 2013a. Studies have shown that in countries with medium HDI, EC is one of the most common cancers Bray et al., 2012. Indeed, EC is more common in less developed or developing countries due to smoking, alcohol consumption, nutritional status, environmental pollution and life style behavior Keramatinia et al., 2016Koca et al., 2015Liu et al., 2014Napier et al., 2014Wang et al., 2015 - combine. HDI is moderate or low in areas with high rates of EC. In these regions, people pay fewer attention to their health and/or are diagnosed late, leading to a lower survival rate for EC compared to people from more developed regions Harirchi et al., 2014Zhang, 2013.
From our analysis, the relationship between the components of the HDI and the incidence of EC revealed that there is a weak negative correlation between life expectancy at birth, mean years of education, and income level with the incidence of EC, but none were statistically significant. However, if we analyze on the basis of gender segregation, the relationship between life expectancy and EC incidence (SIR) in women is significant; this could result from decreased awareness of EC by women and/or fewer health facilities for women than men Kiadaliri, 2014. Other studies have shown that with increasing awareness level, the incidence of risky behaviors such as smoking, physical inactivity, alcohol consumption, and other unhealthy lifestyle associated factors decreases. This, in turn, can affect the incidence of non-communicable diseases such as cancer Castro et al., 2014Koca et al., 2015. Moreover, educated people are more inclined to check on their health status leading to diagnosis and treatment of diseases such as cancer Forbes et al., 2013Mai et al., 2014.
The results of our study also showed that there is a significant negative relationship between the standardized mortality rate of EC (SMR) and HDI. This relationship was significant for life expectancy but not significant for average years of education or income level. Interestingly, similar to SIR of EC, the relationship between life expectancy at birth and SMR of EC in women was significant, but not significant in men. Statistics have shown that the greatest SMR for EC were seen in Malawi, Turkmenistan and Kenya, respectively. A study which examined the role of the Development Index and EC in Asia also obtained similar results to our study Pakzad et al., 2016. Moreover, other studies have shown that the mortality rate of EC in developing countries is higher than in developed ones Lin et al., 2013Torre et al., 2015.
The greater the HDI, the lower the incidence of EC Ferlay et al., 2015Malik, 2013a. In developing and less developed countries, the death rate from cancer will be higher due to weak economic conditions, greater tobacco use, poor diet, greater alcohol consumption, higher incidence of other cancers and, most importantly, lack of adequate access to diagnostic and treatment facilities Liu et al., 2014Mao et al., 2011Rezaianzadeh et al., 2016Rezaianzadeh et al., 2017. Conversely, incidence of some cancers, such as EC, was reduced in developed countries due to better treatment methods, better lifestyle screening, lower risk of infectious diseases, and better access to health care services Lin et al., 2013Mai et al., 2014Salehi et al., 2013Spechler, 2013. Moreover, in countries with better economic and social conditions, and particularly access to earlier diagnosis of diseases, the survival rate of patients will presumably be greater. These factors account for the differences between the incidence and mortality rates of EC in different countries of the world Kiadaliri, 2014Kim et al., 2014Napier et al., 2014.
In ecological studies, such as this one, the results are meant to represent the general population. However, one main limitation is the ecological fallacy can occur, such as when results obtained from the group level are interpreted at the individual level.
Conclusion
The incidence and mortality rates of EC in less developed and developing countries are high. No statistically significant relationship was seen between the standardized incidence and mortality rates of EC and the 2012 HDI.
Abbreviations
ASIR age-standardized incidence rate
ASMR age-standardized mortality rate
EC esophageal cancer
HDI Human Development Index
Author Contribution
All authors contributed to the design of the research. SH, AMH, HS and MG collected the data. SH and AMH conducted analysis and interpretation of data. All authors drafted the first version. SH, AMH and HS edited the first draft. All authors reviewed and commented on final draft.
References
-
F.
Bray,
A.
Jemal,
N.
Grey,
J.
Ferlay,
D.
Forman.
Global cancer transitions according to the Human Development Index (2008-2030): A population-based study . The Lancet Oncology.
2012;
13(8)
:
790-801
.
PubMed View Article Google Scholar -
C.
Castro,
C.
Bosetti,
M.
Malvezzi,
P.
Bertuccio,
F.
Levi,
E.
Negri,
N.
Lunet.
Patterns and trends in esophageal cancer mortality and incidence in Europe (1980-2011) and predictions to 2015 . Annals of Oncology.
2014;
25(1)
:
283-290
.
PubMed View Article Google Scholar -
W.
Chen,
R.
Zheng,
H.
Zeng,
S.
Zhang,
J.
He.
Annual report on status of cancer in China, 2011 . Chinese Journal of Cancer Research.
2015;
27(1)
:
2-12
.
PubMed View Article Google Scholar -
N. A.
Dar,
I. A.
Shah,
G. A.
Bhat,
M. A.
Makhdoomi,
B.
Iqbal,
R.
Rafiq,
P.
Boffetta.
Socioeconomic status and esophageal squamous cell carcinoma risk in Kashmir, India . Cancer Science.
2013;
104(9)
:
1231-1236
.
PubMed View Article Google Scholar -
B. J.
Di Pardo,
N. W.
Bronson,
B. S.
Diggs,
C. R. Jr.
Thomas,
J. G.
Hunter,
J. P.
Dolan.
The global burden of esophageal cancer: A disability-adjusted life-year approach . World Journal of Surgery.
2016;
40(2)
:
395-401
.
PubMed View Article Google Scholar -
J. S. I.
Ferlay,
M.
Ervik.
GLOBOCAN 2012 v1.0. GLOBOCAN, 2012, v10.
2013
.
-
J.
Ferlay,
I.
Soerjomataram,
R.
Dikshit,
S.
Eser,
C.
Mathers,
M.
Rebelo,
F.
Bray.
Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012 . International Journal of Cancer.
2015;
136(5)
:
E359-E386
.
PubMed View Article Google Scholar -
L. J.
Forbes,
A. E.
Simon,
F.
Warburton,
D.
Boniface,
K. E.
Brain,
A.
Dessaix,
J.
Wardle,
the International Cancer Benchmarking Partnership Module 2 Working Group.
Differences in cancer awareness and beliefs between Australia, Canada, Denmark, Norway, Sweden and the UK (the International Cancer Benchmarking Partnership): Do they contribute to differences in cancer survival? . British Journal of Cancer.
2013;
108(2)
:
292-300
.
PubMed View Article Google Scholar -
M.
Ghoncheh,
M.
Mirzaei,
H.
& Salehiniya.
Incidence and mortality of breast cancer and their relationship with the human development index (HDI) in the world in 2012 . Asian Pacific Journal of Cancer Prevention.
2015a;
16(18)
:
8439-8443
.
PubMed View Article Google Scholar -
M.
Ghoncheh,
A.
Mohammadian-Hafshejani,
H.
Salehiniya.
Incidence and mortality of breast cancer and their relationship to development in Asia . Asian Pacific Journal of Cancer Prevention.
2015b;
16(14)
:
6081-6087
.
PubMed View Article Google Scholar -
I.
Harirchi,
S.
Kolahdoozan,
S.
Hajizadeh,
F.
Safari,
Z.
Sedighi,
A.
Nahvijou,
K.
Zendehdel.
Esophageal cancer in Iran; a population-based study regarding adequacy of cancer surgery and overall survival . [EJSO] European Journal of Surgical Oncology.
2014;
40(3)
:
352-357
.
PubMed View Article Google Scholar -
S.
Hassanipour-Azgomi,
A.
Mohammadian-Hafshejani,
M.
Ghoncheh,
F.
Towhidi,
S.
Jamehshorani,
H.
Salehiniya.
Incidence and mortality of prostate cancer and their relationship with the Human Development Index worldwide . Prostate International.
2016;
4(3)
:
118-124
.
PubMed View Article Google Scholar -
A.
Keramatinia,
S.
Hassanipour,
M.
Nazarzadeh,
M.
Wurtz,
A. B.
Monfared,
M.
Khayyamzadeh,
A.
Mosavi-Jarrahi.
Correlation between nitrogen dioxide as an air pollution indicator and breast cancer: A systematic review and meta-analysis . Asian Pacific Journal of Cancer Prevention.
2016;
17(1)
:
419-424
.
PubMed View Article Google Scholar -
A. A.
Kiadaliri.
Gender and social disparities in esophagus cancer incidence in Iran, 2003-2009: A time trend province-level study . Asian Pacific Journal of Cancer Prevention.
2014;
15(2)
:
623-627
.
PubMed View Article Google Scholar -
D. H.
Kim,
E. J.
Gong,
H.-Y.
Jung,
H.
Lim,
J. Y.
Ahn,
K.-S.
Choi,
S.
Baek.
Clinical significance of intensive endoscopic screening for synchronous esophageal neoplasm in patients with head and neck squamous cell carcinoma . Scandinavian Journal of Gastroenterology.
2014;
49 (12)
:
1486-1492
.
PubMed View Article Google Scholar -
T.
Koca,
D.
Arslan,
H.
Basaran,
A. K.
Cerkesli,
D.
Tastekin,
D.
Sezen,
M.
Ozdogan.
Dietary and demographical risk factors for oesophageal squamous cell carcinoma in the Eastern Anatolian region of Turkey where upper gastrointestinal cancers are endemic . Asian Pacific Journal of Cancer Prevention.
2015;
16(5)
:
1913-1917
.
PubMed View Article Google Scholar -
Y.
Lin,
Y.
Totsuka,
Y.
He,
S.
Kikuchi,
Y.
Qiao,
J.
Ueda,
H.
Tanaka.
Epidemiology of esophageal cancer in Japan and China . Journal of Epidemiology.
2013;
23(4)
:
233-242
.
PubMed View Article Google Scholar -
X.
Liu,
X.
Wang,
S.
Lin,
J.
Yuan,
I. T.
Yu.
Dietary patterns and oesophageal squamous cell carcinoma: A systematic review and meta-analysis . British Journal of Cancer.
2014;
110(11)
:
2785-2795
.
PubMed View Article Google Scholar -
P. L.
Mai,
S. T.
Vadaparampil,
N.
Breen,
T. S.
McNeel,
L.
Wideroff,
B. I.
Graubard.
Awareness of cancer susceptibility genetic testing: The 2000, 2005, and 2010 National Health Interview Surveys . American Journal of Preventive Medicine.
2014;
46(5)
:
440-448
.
PubMed View Article Google Scholar -
K.
Malik.
Human development report 2013. The rise of the South: Human progress in a diverse world.
2013a
.
-
K.
Malik.
Summary Human Development Report 2013. The rise of the South: Human progress in a diverse world.
2013b
.
-
W. M.
Mao,
W. H.
Zheng,
Z. Q.
Ling.
Epidemiologic risk factors for esophageal cancer development. Asian Pacific Journal of Cancer Prevention.
2011;
12(10)
:
2461-2466
.
PubMed Google Scholar -
K. J.
Napier,
M.
Scheerer,
S.
Misra.
Esophageal cancer: A Review of epidemiology, pathogenesis, staging workup and treatment modalities . World Journal of Gastrointestinal Oncology.
2014;
6(5)
:
112-120
.
PubMed View Article Google Scholar -
R.
Pakzad,
A.
Mohammadian-Hafshejani,
B.
Khosravi,
S.
Soltani,
I.
Pakzad,
M.
Mohammadian,
Z.
Momenimovahed.
The incidence and mortality of esophageal cancer and their relationship to development in Asia. Annals of Translational Medicine.
2016;
4(2)
:
29
.
PubMed Google Scholar -
A.
Pennathur,
M. K.
Gibson,
B. A.
Jobe,
J. D.
& Luketich.
Oesophageal carcinoma . Lancet.
2013;
381(9864)
:
400-412
.
PubMed View Article Google Scholar -
S.
Razi,
M.
Ghoncheh,
A.
Mohammadian-Hafshejani,
H.
Aziznejhad,
M.
Mohammadian,
H.
Salehiniya.
The incidence and mortality of ovarian cancer and their relationship with the Human Development Index in Asia. ecancermedicalscience.
2016;
10
.
-
A.
Rezaianzadeh,
S. H.
Azgomi,
A. M.
Mokhtari,
A.
Maghsoudi,
M.
Nazarzadeh,
S. L.
Dehghani,
S. R.
Kazerooni.
The Incidence of Breast Cancer in Iran: A Systematic Review and Meta-Analysis . Journal of Analytical Oncology.
2016;
5(4)
:
139-145
.
View Article Google Scholar -
A.
Rezaianzadeh,
M.
Jalali,
A.
Maghsoudi,
A. M.
Mokhtari,
S. H.
Azgomi,
S. L.
Dehghani.
The overall 5-year survival rate of breast cancer among iranian women: A systematic review and meta-analysis of published studies . Breast Disease.
2017;
:
1-6
.
PubMed View Article Google Scholar -
M.
Salehi,
M.
Moradi-Lakeh,
M. H.
Salehi,
M.
Nojomi,
F.
Kolahdooz.
Meat, fish, and esophageal cancer risk: A systematic review and dose-response meta-analysis . Nutrition Reviews.
2013;
71(5)
:
257-267
.
PubMed View Article Google Scholar -
S. J.
Spechler.
Barrett esophagus and risk of esophageal cancer: A clinical review . Journal of the American Medical Association.
2013;
310(6)
:
627-636
.
PubMed View Article Google Scholar -
L. A.
Torre,
F.
Bray,
R. L.
Siegel,
J.
Ferlay,
J.
Lortet-Tieulent,
A.
Jemal.
Global cancer statistics, 2012 . CA: a Cancer Journal for Clinicians.
2015;
65(2)
:
87-108
.
PubMed View Article Google Scholar -
S. B.
Umar,
D. E.
Fleischer.
Esophageal cancer: Epidemiology, pathogenesis and prevention . Nature Reviews. Gastroenterology & Hepatology.
2008;
5(9)
:
517-526
.
PubMed View Article Google Scholar -
N.
Wang,
F.
Cao,
F.
Liu,
Y.
Jia,
J.
Wang,
C.
Bao,
Y.
Cheng.
The effect of socioeconomic status on health-care delay and treatment of esophageal cancer . Journal of Translational Medicine.
2015;
13(1)
:
241
.
PubMed View Article Google Scholar -
X.
Wang,
J.-C.
Fan,
A.-R.
Wang,
Y.
Leng,
J.
Li,
Y.
Bao,
Y.
Ren.
Epidemiology of esophageal cancer in Yanting - regional report of a national screening programme in China . Asian Pacific Journal of Cancer Prevention.
2013;
14(4)
:
2429-2432
.
PubMed View Article Google Scholar -
W.-Q.
Wei,
Z.-F.
Chen,
Y.-T.
He,
H.
Feng,
J.
Hou,
D.-M.
Lin,
Y. L.
Qiao.
Long-term follow-up of a community assignment, one-time endoscopic screening study of esophageal cancer in China . Journal of Clinical Oncology.
2015;
33(17)
:
1951-1957
.
PubMed View Article Google Scholar -
Y.
Zhang.
Epidemiology of esophageal cancer . WJG.
2013;
19(34)
:
5598-5606
.
PubMed View Article Google Scholar
Comments

Downloads
Article Details
Volume & Issue : Vol 4 No 9 (2017)
Page No.: 1607-1623
Published on: 2017-09-20
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 5956 times
- Download PDF downloaded - 1451 times
- View Article downloaded - 4 times
 Biomedpress
Biomedpress