Abstract
Multiple myeloma is described by the proliferation of malignant plasma cells, in which orbital involvement is rare. In this report, we collected all cases with orbital multiple myeloma from 2009 to 2018 and investigated the characteristics such as sex, age, common orbital symptoms, unilateral or bilateral and different therapeutic options. Also, we reported an uncommon case of multiple myeloma that has been developed into plasmacytoma. Our patient had been initially diagnosed with multiple myeloma, but after a few months, the disease had progressed to secondary extramedullary plasmacytoma in the retrobulbar. Therapeutic measures, such as surgery to prevent its development in the patient's eye, were successful.
Introduction
Multiple myeloma is a tumor of malignant plasma cells that consider as the second most common hematologic malignancy 1. This disease has an age-adjusted incidence of 4.7 cases per 100,000 populations 2. It often occurs in adults, and the mean age at diagnosis is 70 years 3. One of the most prominent features of this disorder is the presence of more than 10% clonal plasma cells in the bone marrow or biopsy associated with end-organ damage 2. Also, in 1846, Dalrymple and Bence Jones discovered an uncommon plasma cell tumor known as plasmacytoma 4. The etiology of plasmacytoma remains largely unknown, but factors such as viral pathogenesis have been identified and genetic factors may also be involved 5. The purpose of this paper is to report a 62-year-old man with a clinical and pathological history of multiple myeloma, who presented evidence of a mass in the retrobulbar area of the eye.
Case Presentation
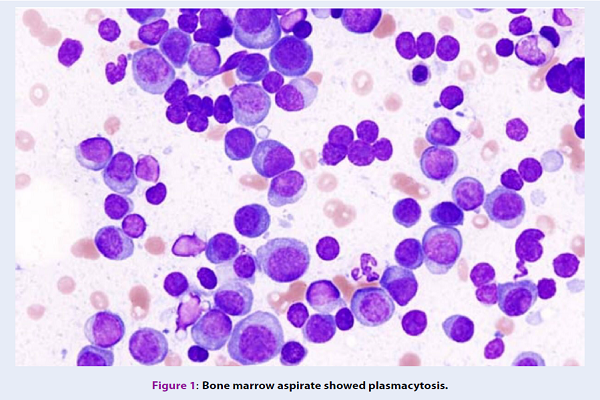
In January 2018, a 62-year-old man was referred to our Clinic of Hematology and oncology, with one week of back pain history, and loss of consciousness in the neurological examination. Further analysis revealed the symptom of kidney failure. In primary laboratory investigations, he had normocytic normochromic anemia with Hb: 9.6g/dL, normal WBC and a decrease in platelet count (WBC: 8,300/mm3; Platelet count: 79,000/mm3). Also, renal function tests (RFT) and serum electrolytes were usually performed in multiple myeloma. The results of these tests showed hypergammaglobulinemia (5g/dL) and an increase in blood urea nitrogen (BUN) and serum creatinine (Cr) levels (BUN 64 mg/dL, Cr 8.1 mg /dL). Magnetic resonance imaging of the lumbar spine indicated vertebral collapse at T12 and L2. Examination of the bone marrow aspiration (BMA) and bone marrow biopsy revealed that a high percentage of plasma cells (>20% plasma cells) were negative for CD19, and positive for CD38, CD138 (Figure 1).
Our diagnosis was multiple myeloma and immediately started treatment with bortezomib, cyclophosphamide, and dexamethasone (the approved VCD is preferable as induction therapy for newly diagnosed multiple myeloma especially with renal failure). Also, zoledronic acid was used to reduce bone pain.
After 6 cycles, the initial response to treatment was relatively good. Five months later, the patient referred to an ophthalmologist with symptoms such as swelling of the right eyelid with ptosis, diplopia and blurred vision. In fundus examination, few scattered hemorrhages were seen in the left eye and the results of Visual Acuity for this eye were as follows: OD: 6/10, OS: 4/10. Also, the results of orbit computed tomography (CT) demonstrated a soft tissue mass (26 × 12 mm) in the retrobulbar of the left eye (Figure 2). In fine needle aspiration cytology (FNAC) of the mass, mature and immature plasma cells were observed, which led to the diagnosis of secondary extramedullary plasmacytoma. Thus, the patient underwent surgical debulking, the lesion was removed from the retrobulbar area and the result was successful. Currently, the patient’s condition is good, and he is continuing chemotherapy cycles with bortezomib and dexamethasone.
Discussion
Plasmacytoma, as an unusual tumor of malignant plasma cells, indicates 5-10% of all plasma cell neoplasms 6 and plasmacytoma can occur as a primary or secondary tumor, based on the presence or absence of systemic disease 7. Also, these neoplasms are divided into four different types: solitary plasmacytoma of bone (SPB), extramedullary plasmacytoma (EMP), multiple myeloma (MM) and plasma cell leukemia 8. The organs involved in the SPB are mainly axial skeletal bones, such as vertebra and skull, while in EMP, the head and neck, nasal cavity and nasopharyngeal are commonly involved 6. It has been reported that the rate of relapse after treatment for extramedullary plasmacytoma is 6-10% 9.
Also, MM is characterized by the proliferation of abnormal plasma cells and is usually limited to bone marrow 10. Extramedullary plasmacytoma has been reported in 3% of patients with MM 11. In these patients, orbital involvement is rare. According to the study performed by Burkat and colleagues 12, from 1972 to 2009, 52 cases of orbital multiple myeloma with a mean age of 56.5 have been reported and in 81% of them, the most common symptom was proptosis. Based on our reviews, from 2010 to 2018, about 20 cases have been described, which are listed in Table 1.
The mean age of these patients was 63.8 and in the many cases, orbital symptom has been unilateral (85%). The proptosis and diplopia were the most abundant orbital clinical symptoms involved, while ptosis, retrobulbar lesion, and low vision were less common (Table 2). Also, systemic chemotherapy and radiotherapy are good therapeutic options that in the most reports, the positive response to treatment has been reported 13. We reported a multiple myeloma patient with extramedullary plasmacytoma that was unique because of the unilateral retrobulbar lesion and its successful orbital surgery.
| Author (yr) | # Cases | Age (yr) | Sex | Orbital Symptoms | Unilateral vs Bilateral | Typical management | Ref. |
| Burkat (2009) | 1 | 65 | M | decreased vision andeyelid pain | Unilateral | Orbital surgery and chemotherapy | 12 |
| Yumori (2010) | 1 | 33 | M | Vascularized conjunctival lesion | Bilateral | Ophthalmic solution and prednisolone acetate | 7 |
| Fernandez (2011) | 1 | 53 | M | Moderate ptosis and hypotropia | Unilateral | Chemotherapy treatment and autologous bone marrow transplantation | 14 |
| Chin (2011) | 3 | 82, 76, 76 | 1F,2M | Epibulbar lesion and proptosis | Unilateral | Palliative radiotherapy and chemotherapy(melphalan and prednisone) | 15 |
| Liao (2011) | 1 | 53 | F | Left globe proptosis | Unilateral | Ocular surface lubrication | 16 |
| Pan (2011) | 1 | 57 | F | Right eye proptosis | Unilateral | Pamidronate chemotherapy and orbital radiotherapy | 17 |
| Terenzi (2012) | 1 | 50 | M | Retro-orbital lesion | Unilateral | Intensity-modulated radiotherapy technique (IMRT) | 3 |
| Hassan (2012) | 1 | 62 | F | Proptosis, chemosis, diplopia and decreased vision | Unilateral | Radiotherapy | 13 |
| Felici (2013) | 1 | 73 | M | Retro-orbital localization | Bilateral | Combination chemotherapy (lenalidomide,dexamethasone, and cyclophosphamide) | 18 |
| Varım (2015) | 1 | 64 | M | Peri-orbital ecchymosis lesion (raccoon eye) | Unilateral | Combination chemotherapy (VAD and VCD) | 19 |
| Galea (2015) | 1 | 58 | F | Diplopia and variable Ptosis | Bilateral | CombinationDexamethasone) | 20 |
| Vatansever (2016) | 1 | 68 | F | Right eye proptosis | Unilateral | Palliative radiotherapy | 21 |
| Nambiar (2017) | 1 | 63 | F | Ptosis and diplopia | Unilateral | Chemotherapy (bortezomib, lenalidomide, and dexamethasone) | 22 |
| Wang (2018) | 5 | 68, 73, 51, 77,75 | 3F, 2M | The retrobulbar lesion, diplopia, and proptosis | Unilateral | Orbital surgery in conjunction with radiotherapy and chemotherapy | 11 |
| Characteristics | N: 20 |
| Age | 63.8 |
| Sex | 10 M (50%), 10 F (50%) |
| Unilateral vs Bilateral | 3 Bil (15%), 17 Uni (85%) |
| Common orbital symptoms | Proptosis: 12 (60%)Retro-bulbar (-orbital) lesion: 3 (15%) |
Conclusion
According to studies conducted to date, in patients with multiple myeloma, orbital symptoms often occur in adulthood and unilaterally. Additionally, the important point in these cases is that during differential diagnosis between the types of plasmacytomas, initially multiple myeloma should be considered.
List of abbreviations
BMA: bone marrow aspiration
BUN: blood urea nitrogen
CBC: complete blood count
Cr: creatinine
CT: computed tomography
EMP: extramedullary plasmacytoma
FNAC: fine needle aspiration cytology
MM: multiple myeloma
RFT: renal function tests
SPB: solitary plasmacytoma of bone
VCD: velcade (bortezomib), cyclophosphamide, and dexamethasone
Ethics approval and consent to participate
Yes
Competing interests
The authors declare that they have no financial or other conflicts of interest.
Funding
None.
Authors’ contributions
Mehrdad Payandeh & Noorodin Karami: Literature search, Clinical studies, Data acquisition, Data analysis;
Noorodin Karami: Manuscript preparation, Manuscript review, Guarantor;
Afshin Karami: Concepts, Design, Definition of intellectual content, Literature search, Manuscript editing;
Soode Enayati, Fatemeh Yari & Mehrnoush Aeinfar: Manuscript editing, Literature search.
References
-
Burkat
C. N.,
Van Buren
J. J.,
Lucarelli
M. J..
Characteristics of orbital multiple myeloma: a case report and literature review. Survey of Ophthalmology.
2009;
54
:
697-704
.
-
Wang
S. S.,
Lee
M. B.,
George
A.,
Wang
S. B.,
Blackwell
J.,
Moran
S..
Five cases of orbital extramedullary plasmacytoma: diagnosis and management of an aggressive malignancy. Orbit (Amsterdam, Netherlands).
2018;
(7)
:
1-8
.
-
Nambiar
R. K.,
Nair
S. G.,
Mathew
S. P.,
Manohar
A. T..
Ptosis and diplopia—sole manifestations in multiple myeloma. Annals of Blood.
2017;
2
:
9
.
-
Vatansever
M.,
Bozkurt
F. M.,
Dinç
E.,
Yılmaz
E. B.,
Nayir
E.,
Sarı
A. A..
Orbital metastasis of multiple myeloma: case report. Turkish Journal of Ophthalmology.
2016;
46
:
148-50
.
-
Galea
Martin,
McMillan
Nigel,
Weir
Clifford.
Diplopia and variable ptosis as the sole initial findings in a case of orbital plasmacytoma and multiple myeloma. Seminars in ophthalmology.
2015;
30
:
235-237
.
-
Varım
C.,
Ergenc
H.,
Uyanık
M. S.,
Kaya
T.,
Nalbant
A.,
Karacaer
C..
A very rare presentation of multiple myeloma: unilateral raccoon eye. Open Access Macedonian Journal of Medical Sciences.
2015;
3
:
436-8
.
-
Felici
S,
Villivà
N,
Balsamo
G,
Andriani
A.
Efficacy of lenalidomide in association with cyclophosphamide and dexamethasone in multiple myeloma patient with bilateral retro-orbital localisation. ecancermedicalscience.
2013;
7
:
331
.
-
Hassan
Mona,
Alirhayim
Zaid,
Sroujieh
Laila,
Hassan
Syed.
Multiple myeloma of the orbit. Case reports in ophthalmological medicine.
2012;
2012
.
-
Terenzi
S.,
di Cristino
D.,
Murgia
A.,
Janniello
D.,
Ponti
E.,
Tolu
B..
Orbital Involvement in Multiple Myeloma: A Case Report. Journal of Cancer Therapy.
2012;
3
:
1052-4
.
-
Pan
S. W.,
Hitam
W. H. Wan,
Noor
R. A. Mohd,
Bhavaraju
V. M..
Recurrence of multiple myeloma with soft tissue plasmacytoma presenting as unilateral proptosis. Orbit (Amsterdam, Netherlands).
2011;
30
:
105-7
.
-
Liao
J.,
Greenberg
A.,
Shinder
R..
Relapsed multiple myeloma presenting as an orbital plasmacytoma. Ophthalmic Plastic and Reconstructive Surgery.
2011;
27
:
461
.
-
Chin
K. J.,
Kempin
S.,
Milman
T.,
Finger
P. T..
Ocular manifestations of multiple myeloma: three cases and a review of the literature. Optometry (St. Louis, Mo.).
2011;
82
:
224-30
.
-
Fernandez‐Perez
S.,
Satue
M.,
Latorre
R. Herrero,
Mata
G. De La,
Idoipe
M.,
Garcia‐Martin
E..
Orbital involvement in multiple myeloma. Acta Ophthalmologica.
2011;
Special issue: Abstracts from the 2011 European Association for Vision and Eye Research Conference
:
89
.
-
Yumori
J. W.,
Ilsen
P.,
Bright
D. C..
Conjunctival plasmacytoma. Optometry (St. Louis, Mo.).
2010;
81
:
234-9
.
-
Köhler
M.,
Greil
C.,
Hudecek
M.,
Lonial
S.,
Raje
N.,
Wäsch
R..
Current developments in immunotherapy in the treatment of multiple myeloma. Cancer.
2018;
124
:
2075-85
.
-
Breen
D. P.,
Freeman
C. L.,
De Silva
R. N.,
Derakhshani
S.,
Stevens
J..
Soft tissue plasmacytomas in multiple myeloma. Lancet.
2017;
390
:
2083
.
-
Clamp
J. R..
Some aspects of the first recorded case of multiple myeloma. Lancet.
1967;
2
:
1354-6
.
-
Weber
D. M..
Solitary bone and extramedullary plasmacytoma. Hematology.
2005;
2005
:
373-6
.
-
Kilciksiz
Sevil,
Karakoyun-Celik
Omur,
Agaoglu
Fulya Yaman,
Haydaroglu
Ayfer.
A review for solitary plasmacytoma of bone and extramedullary plasmacytoma. The Scientific World Journal.
2012;
2012
.
-
Townend
P. J.,
Kraus
G.,
Coyle
L.,
Nevell
D.,
Engelsman
A.,
Sidhu
S. B..
Bilateral extramedullary adrenal plasmacytoma: case report and review of the literature. International Journal of Endocrine Oncology.
2017;
4
:
67-73
.
-
Lim
C. C.,
Soong
T. K.,
Chuah
K. C.,
Subrayan
V..
Extramedullary plasmacytoma of the eyelid: a case report and review of literature. Clinical & Experimental Optometry.
2013;
96
:
349-51
.
-
Payandeh
M.,
Karami
N.,
Karami
A.,
Aeinfar
M.,
Yami
A.,
Ghorbani
S..
A Good Therapeutic Strategy to Unrecognized HIV Infection in A Patient with Multiple Myeloma Undergoing Peripheral Blood Stem Cell Transplantation-Case Report. The American Journal of Cancer.
2018;
6
:
17-9
.
Comments
Downloads
Article Details
Volume & Issue : Vol 5 No 9 (2018)
Page No.: 2703-2707
Published on: 2018-09-29
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 5875 times
- Download PDF downloaded - 1284 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress



