Abstract
Background & Aim: Drug abusers have much lower pain threshold, in a way that the duration of the effect of anesthesia on controlling their pain is still not fully known. Therefore, this study aimed to compare the duration of spinal anesthesia induced with bupivacaine between drug-dependent and non-dependent individuals.
Methods: This quasi-experimental study was conducted on two 60-member groups consisting of drug-dependent and non-dependent patients undergoing lowerlimb orthopedic surgery. Patients were selected via simple convenience sampling and underwent a similar procedure of spinal anesthesia using the same needle and medicine by an anesthesiologist, who was unaware of the patients' placement in the study groups. After surgery, the duration of patients' anesthesia was correspondingly measured in both groups and compared using the independent t-test.
Results: In this research study, no significant difference was observed between the groups in terms of age and gender. The mean duration of opium abuse in the drug-dependent patient group was reported to be 7.5+/-1.3 years. In addition, the duration of spinal anesthesia in the drug-dependent patient group was shorter, compared to the non-dependent group (P=0.0001).
Conclusion: According to the results of the study, intrathecal bupivacaine is not a durable anesthesia, for performing surgeries that might last more than an hour, in drug-dependent patients.
Introduction
Long-term drug abuse can result in increased drug dose to achieve analgesic effects. This process is called drug tolerance syndrome and its mechanism is not completely understood 12.
However, some hypotheses have been put forth explaining that the shape and function of receptors are likely to change as the drug concentration varies 2.
Considering legal limitations and social stigma, no accurate statistics on drug addiction have been reported in Iran. Nonetheless, inhalant abuse is the most common method of drug abuse in this country 34.
A shorter duration of spinal anesthesia was observed in chronic drug abusers, compared to non-dependent individuals, as reported by Dabbagh and colleagues; the researchers suggested comparing the levels of spinal anesthesia between the two groups in future studies 5.
While local anesthesia with bupivacaine acts through blocking sodium channels 6, drugs exert their analgesic effects via µ receptors 7.
There is similar mild respiratory acidosis among drug abusers. These individuals experience hypo ventilation since acidosis may cause hydrogen (H+) entry into cerebrospinal fluid, subsequently decreasing the impact of anesthetics. These observations strongly suggest that there is a resistance to local anesthesia among drug-dependent individuals. Nevertheless, this hypothesis can be challenging to prove and further studies are required in this regard 89.
With this background in mind, the aim of this study was to compare the duration of spinal anesthesia with bupivacaine between drug-dependent and non-dependent patients.
Methods
Study Design and Ethical principles
This quasi-experimental study was conducted on 120 patients referred to Khatam al-Anbiya Hospital in Zahedan, Iran to undergo lower-limb orthopedic surgery. The research was approved by the Vice-Chancellor’s Office for Research and the Ethics Committee of Zahedan University of Medical Sciences. In addition, an informed consent was obtained from all participants.
Patients and Sample Size
The subjects were selected via simple convenience sampling. In this regard, all candidates for lower-limb orthopedic surgery were enrolled in the study after meeting the inclusion criteria. Following that, the participants were divided into two 60-member groups of drug-dependent and non-dependent patients, in accordance with their history of drug abuse. Similarly, the sample size was estimated at 120 with reference to the relevant literature and based on the sample size calculation formula 5.
Inclusion and Exclusion Criteria
The inclusion criteria included the age range of 20-50 years, possibility of using spinal anesthesia for the person, lack of coagulation disorders, no history of cardiovascular diseases, no diabetes, no diseases leading to neuropathy, no simultaneous addiction to non-opioids, lack of backbone disorders, no head trauma with high intracranial pressure, fracture of a lower limb, and patient’s willingness to participate in the study. The exclusion criteria were lack of willingness to cooperate with the researcher, failure of spinal anesthesia and the need to have general anesthesia, feeling pain during the surgery, and the need to inject narcotics during the surgery.
Interventions
One day before the surgery, an anesthesiologist (the researcher) visited all patients and cardiovascular counseling, along with echocardiography, was conducted for all of patients after the visit. To alleviate pain in the drug-dependent patients prior to surgery, they were allowed to use their typical narcotics with their routine methods. In addition, 5 mg of morphine was injected intramuscularly in the gluteal muscle if the pain was persistent. It should be noted that just 5 mg of intramuscular morphine was injected into the non-dependent group, and only in the presence of pain. Since patients must fast for 8 hours before to surgery (NPO: nil per os/nothing by mouth), the infusion of 10 cc/kg of dextrose saline serum was started from the beginning of NPO and continued until the onset of the surgery. At the beginning of the surgery, the infusion of 10 cc/kg of serum ringer was initiated through the peripheral veins, followed by pulse oximetry screening and cardiac monitoring. After that, 4 cc of 0.5% bupivacaine (20 mg) was injected by needle (No. 25) between vertebrae L3-L4 in the subarachnoid space under sterilized conditions in a sitting position by an anesthesiologist, who was unaware of the patients’ placement in the study groups.
In the next stage, the participants were put in the dorsal recumbent position and were intravenously administered with 2 mg of midazolam for sedation. In addition, mask oxygen therapy was performed at 6 L/min. After 5 minutes, the pinprick test was performed to confirm the effectiveness of spinal anesthesia. The given test was repeated every 10 minutes during the surgery. If the anesthesia was ineffective at any stage of the test, general anesthesia was applied and the patients were excluded from the study. However, if the anesthesia was effective, the patients’ surgery was conducted by an orthopedist, who was unaware of the patients’ placement in the study groups. Following that, the duration of the patients’ anesthesia after the surgery, along with the demographic characteristics and history of drug abuse, were recorded for each patient in pre-designed forms.
Statistical Analysis
Data analysis was performed using the statistics program SPSS (version 24), with descriptive statistics, Chi-square test, and independent t-test.
Results
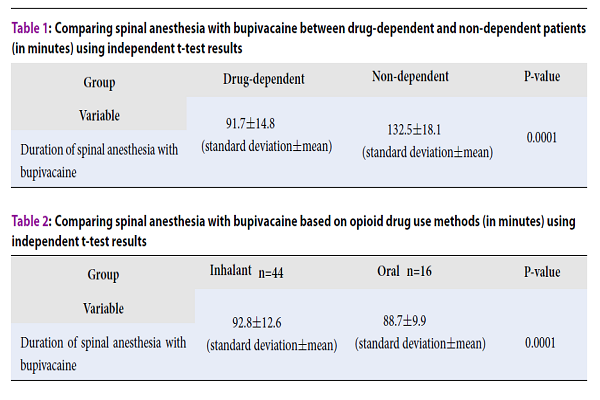
In this research study, 72 (60%) patients were male and 48 (40%) participants were female. According to the results, no significant difference was observed between the study groups in terms of gender, considering the results of the Chi-square (P=0.60). The mean age of the patients was 37.4±5.7 years, wherein there were 16 (13.3%), 69 (57.5%), and 35 (29.2%) individuals in the age groups of 20-30, 30-40, and 40-50 years, respectively. Moreover, no significant difference was observed in the mean age of the study groups (P=0.863). On the other hand, the mean duration of drug abuse in the drug-dependent group was reported to be 7.5±1.3 years. Furthermore, 44 (73.3%) and 16 (26.7%) of the participants had a history of drug abuse in inhalant and oral forms, respectively. Comparison of the spinal anesthesia duration between the two groups indicated a shorter period in the drug-dependent patient group, as compared to the other patient group (non-dependent). In addition, the effect of spinal anesthesia in these patients was eliminated earlier, and this difference was statistically significant (Table 1).
| Group/Variable | Drug-dependent | Non-dependent | P-value |
| Duration of spinal anesthesia with bupivacaine | 91.7±14.8(standard deviation±mean) | 132.5±18.1(standard deviation±mean) | 0.0001 |
From comparison of results based on the type of drug intake (oral versus inhalant), it was demonstrated that in inhalant abusers, spinal anesthesia was higher, as compared to oral drug users. While there was a slight difference in the mean duration, it was statistically significant (Table 2).
| Group/Variable | Inhalantn=44 | Oral n=16 | P-value |
| Duration of spinal anesthesia with bupivacaine | 92.8±12.6 (standard deviation±mean) | 88.7±9.9 (standard deviation±mean) | 0.0001 |
Discussion
The results of this study showed that the duration of spinal anesthesia was significantly shorter in the drug-dependent patients, compared to the non-dependent individuals. It should be noted that the effect of narcotic compounds on the body’s pain system can be induced not only by conventional opioid receptors but by other numerous receptors in the central and peripheral nervous systems, which can be significantly affected by such compositions 10. Among chronic drug abusers, the responses of opioid receptors to painful stimuli fluctuate. In this respect, frequent substance abuse can lead to a connection between opioids and receptors, thereby preventing the proper transcription of DNA and production of non-natural proteins, which can result in hyperalgesia and allodynia 111121314.
Moreover, the immune response of such patients is altered and there is an increase in the ratio of pro-inflammatory interleukins to anti-inflammatory interleukins.
These above factors suggest a decrease in the relative effect of anesthesia medications during surgery as well as the potential need for a higher dose of medicine to control the patients’ pain and stress. As these have not been proven, further studies would be helpful in this regard 15161718. In a study by Sadeghi et al., the duration of spinal anesthesia in drug-dependent and non-dependent patients was measured. Sadeghi et al. divided the subjects into four groups. In the first group, consisting of non-dependent individuals, hyperbaric bupivacaine with 1 cc of saline was injected; in the second group encompassing non-dependent patients, bupivacaine with sufentanil was injected; in the third group containing drug-dependent subjects, placebo and intrathecal bupivacaine were injected; and finally in the fourth group (the drug-dependent patients), sufentanil and intrathecal bupivacaine were injected. After that, the start time and duration of anesthesia in the study groups were measured and compared. According to the results, there was a shorter duration of spinal anesthesia in the third group, compared to the other study groups. It was concluded that adding 5 mg of intrathecal sufentanil to the patients’ local anesthesia could make the duration of their spinal anesthesia equivalent to that of non-dependent patients 3.
Despite the difference in the type of drug used in the aforementioned and present studies, our findings are in agreement with the results obtained by Sadeghi and colleagues 3. In line with the results of the present study, Dabbagh et al. (2007) reported that the duration of spinal anesthesia in opioid abusers and control groups were 86.6±15.7 and 162±22.1 minutes, respectively, and that this difference was statistically significant. This study also indicated that the duration of spinal anesthesia with bupivacaine was shorter in the groups of opioid abusers, which was probably due to the cross-resistance between the anesthesia area and the opioid compounds in the spinal neurons 5. In a research by Karbasy et al. (20), however, when the levels and duration of spinal anesthesia with bupivacaine in drug-dependent and non-dependent individuals were compared, a significantly longer duration of spinal anesthesia in drug-dependent patients and lower levels of spinal anesthesia were observed, as compared to non-dependent individuals.
One of the major drawbacks of the study herein was the lack of evaluation of the levels and duration of spinal anesthesia. Nevertheless, the obtained results confirmed that using bupivacaine might be insufficient for inducing anesthesia in drug-dependent individuals 19. Furthermore, in a study by Hashemian et al. on drug-dependent and non-dependent patients with hand injury, it was reported that the drug-dependent patients required higher doses of lidocaine for injury block. In addition, the results were indicative of a significantly longer starting time for these individuals 20. Certainly, one should pay particular attention to the fact that in Iranian culture, it is a social disgrace to admit your addiction. Another major limitation of this study is the reliance of accurate data on self-reporting (especially about addiction). This impacts placement of patients in the correct group (drug-dependent versus non-dependent). For example, a patient may have an addiction to a drug but not find that addiction bothersome; thus, they may be placed wrongly in the non-dependent group as opposed to dependent group. It is also worth noting that patients’ dissatisfaction with performing the addiction test for entering into the study was an unresolved issue, which might have contributed to the distortion of the final results.
Conclusion
According to the results of the study, there was a significantly shorter duration of spinal anesthesia in the drug-dependent individuals, compared to the non-dependent subjects. Therefore, spinal anesthesia can only be used in short-term surgeries for drug dependent people. In general, it is recommended that general anesthesia be used for these patients in surgeries that may last more than an hour.
Competing Interests
The authors declare that there is no conflict of interest regarding the publication of this article.
Funding
The study was financially supported by Zahedan University of Medical Sciences, Zahedan, Iran.
Authors' Contributions
Faranak Beirami: advising in development of research and revising this paper.
Masoum Khoshfetrat: participating in the implementation of research and supervising the data collection and revising the paper.
Hadi Khosravi: participating in the implementation of research and data collection.
Aliakbar Keykha: Compiling and editing the paper. All authors reviewed, commented and approved the final version.
Acknowledgments
This article was extracted from a thesis written by a resident of anesthesiology and critical care, approved and funded by Research and Technology Deputy of Zahedan University of Medical Sciences. Hereby, we extend our gratitude to the Research and Technology Deputy of the University. In addition, we would like to thank the staff and orthopedic surgery ward at the Khatam-ol-Anbia Hospital of Zahedan for assisting us in this research.
References
-
Ossipov
M. H.,
Lai
J.,
King
T.,
Vanderah
T. W.,
Porreca
F..
Underlying mechanisms of pronociceptive consequences of prolonged morphine exposure. Biopolymers.
2005;
80
:
319-24
.
-
Gardell
L. R.,
King
T.,
Ossipov
M. H.,
Rice
K. C.,
Lai
J.,
Vanderah
T. W..
Opioid receptor-mediated hyperalgesia and antinociceptive tolerance induced by sustained opiate delivery. Neuroscience Letters.
2006;
396
:
44-9
.
-
Sadeghi
M.,
Yekta
R. A.,
Azimaraghi
O.,
Barzin
G.,
Movafegh
A..
Evaluation of spinal anesthesia blockade time with 0.5% hyperbaric bupivacaine, with or without sufentanil, in chronic opioid users: a randomized clinical trial. Brazilian Journal of Anesthesiology.
2016;
66
:
346-50
.
-
Mokri
Azarakhsh.
Brief overview of the status of drug abuse in Iran. 2002
.
-
Dabbagh
A.,
Dahi-Taleghani
M.,
Elyasi
H.,
Vosoughian
M.,
Malek
B.,
Rajaei
S..
Duration of spinal anesthesia with bupivacaine in chronic opium abusers undergoing lower extremity orthopedic surgery. Archives of Iranian Medicine.
2007;
10
:
316-20
.
-
Wood
J. N.,
Boorman
J. P.,
Okuse
K.,
Baker
M. D..
Voltage-gated sodium channels and pain pathways. Journal of Neurobiology.
2004;
61
:
55-71
.
-
Gomes
I.,
Jordan
B. A.,
Gupta
A.,
Trapaidze
N.,
Nagy
V.,
Devi
L. A..
Heterodimerization of μ and δ opioid receptors: A role in opiate synergy. The Journal of Neuroscience : The Official Journal of the Society for Neuroscience.
2000;
20
:
RC110
.
-
Kouzehgaran
S.,
Saber-Tanha
A..
What Is the Main Reason for Reduction in Duration of Action of Local Anesthetics Used for Spinal Anesthesia in Opium Addicted Patients?. Addiction & Health.
2015;
7
:
198
.
-
Shook
J. E.,
Watkins
W. D.,
Camporesi
E. M..
Differential roles of opioid receptors in respiration, respiratory disease, and opiate-induced respiratory depression. The American Review of Respiratory Disease.
1990;
142
:
895-909
.
-
Bovill
J. G..
Mechanisms of actions of opioids and non-steroidal anti-inflammatory drugs. European Journal of Anaesthesiology. Supplement.
1997;
15
:
9-15
.
-
King
T.,
Ossipov
M. H.,
Vanderah
T. W.,
Porreca
F.,
Lai
J..
Is paradoxical pain induced by sustained opioid exposure an underlying mechanism of opioid antinociceptive tolerance?. Neuro-Signals.
2005;
14
:
194-205
.
-
Angst
M. S.,
Clark
J. D..
Opioid-induced hyperalgesia: a qualitative systematic review. Anesthesiology.
2006;
104
:
570-87
.
-
Xu
H.,
Xu
T.,
Ma
X.,
Jiang
W..
Involvement of neuronal TGF-β activated kinase 1 in the development of tolerance to morphine-induced antinociception in rat spinal cord. British Journal of Pharmacology.
2015;
172
:
2892-904
.
-
Dogrul
A.,
Bilsky
E. J.,
Ossipov
M. H.,
Lai
J.,
Porreca
F..
Spinal L-type calcium channel blockade abolishes opioid-induced sensory hypersensitivity and antinociceptive tolerance. Anesthesia and Analgesia.
2005;
101
:
1730-5
.
-
King
T.,
Gardell
L. R.,
Wang
R.,
Vardanyan
A.,
Ossipov
M. H.,
Malan
T. P..
Role of NK-1 neurotransmission in opioid-induced hyperalgesia. Pain.
2005;
116
:
276-88
.
-
Vera-Portocarrero
L. P.,
Zhang
E. T.,
King
T.,
Ossipov
M. H.,
Vanderah
T. W.,
Lai
J..
Spinal NK-1 receptor expressing neurons mediate opioid-induced hyperalgesia and antinociceptive tolerance via activation of descending pathways. Pain.
2007;
129
:
35-45
.
-
Xu
Z. Z.,
Kim
Y. H.,
Bang
S.,
Zhang
Y.,
Berta
T.,
Wang
F..
Inhibition of mechanical allodynia in neuropathic pain by TLR5-mediated A-fiber blockade. Nature Medicine.
2015;
21
:
1326-31
.
-
Araldi
D.,
Ferrari
L. F.,
Levine
J. D..
Repeated mu-opioid exposure induces a novel form of the hyperalgesic priming model for transition to chronic pain. The Journal of Neuroscience : The Official Journal of the Society for Neuroscience.
2015;
35
:
12502-17
.
-
Karbasy
S. H.,
Derakhshan
P..
Effects of opium addiction on level of sensory block in spinal anesthesia with bupivacaine for lower abdomen and limb surgery: a case-control study. Anesthesia and Pain Medicine.
2014;
4
:
e21571
.
-
Hashemian
A. M.,
Omraninava
A.,
Kakhki
A. D.,
Sharifi
M. D.,
Ahmadi
K.,
Masoumi
B..
Effectiveness of local anesthesia with lidocaine in chronic opium abusers. Journal of Emergencies, Trauma and Shock.
2014;
7
:
301-4
.
Comments
Downloads
Article Details
Volume & Issue : Vol 5 No 10 (2018)
Page No.: 2721-2725
Published on: 2018-10-15
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 5701 times
- Download PDF downloaded - 1279 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress


