Abstract
Introduction: The current study aims to assess the antinociceptive and anti-inflammatory activities of Amygdalus eburnea Spach extract in mice.
Methods: Totally, 114 NMRI mice were used in this study. The acute toxicity was evaluated for two days. The antinociceptive effect was accessed by using the hot-plate, tail-flick, and rotarod test. In this investigation, anti-inflammatory effects were evaluated by using the Xylene-induced ear edema method. The findings demonstrated that in the hot-plate and tail-flick tests, A. eburnea extract particularly at the dose of 750 mg/kg demonstrated a considerable analgesic effect; so that there was a significant difference between the extract-treated group and the control group (p<0.05).
Results: The results showed that the administration of A. eburnea extract especially at the dose of 500 and 750 mg/kg significantly decreased the ear edema induced by xylene in comparison to the control group. There was no significant difference after injecting of various doses of A. eburnea extract in the sensory-motor test (p > 0.05).
Conclusion: These results demonstrated the potent antinociceptive and anti-inflammatory effects of A. eburnea extract in mice. Nevertheless, the precise mechanisms responsible for these activities remain to be studied.
Introduction
Pain is a complex process and an unpleasant sensory experience that is usually caused by the stimulation of free nerve terminals 1. In another definition, pain can be said to be a vigilant experience that results from brain activity in response to harmful stimuli and involves sensory, emotional and cognitive processes that can lead to isolation, immobility, and drug dependence 12. ain sometimes persists despite the removal of irritants and the improvement in the outlook at the affected sites, but pain usually disappears after the removal of the excitation sources 3. Generally, pain is divided into two categories: (i) acute pains are those usually accompany with ulcers and diseases. Acute pains can be very short and transient, such as an insect bite, or may last for a long time like a burn; (ii) Chronic pains are those last more than six months from its onset, and their termination is not predictable. Unlike acute pains, which causes are usually known, causes for chronic pains may remain unknown 31.
Given that more than 50% of people in the world have experiences with pains, there is a constant quest for effective medications to relieve pains 13. Although chemical drugs that are used today to reduce pains have some desired properties, they have unwanted and harmful effects, such as gastrointestinal bleeding and cardiovascular disorders, which makes the use of these medicines dangerous. Hence, finding alternative solutions which are not only effective in relieving pain but also have minimal side effects is an essential task 456.
For many years, plant materials and derivatives have been considered as alternative approaches to chemical drugs 7. Amygdalus eburnea Spach with the local name “Ghosk”, is a plant of the Rosaceae family. This family includes species that are close to crop almonds and have spread from Central Asia to southern Europe, and southern parts of Iran 8 A. eburnea is in the form of trees or shrubs without thorns or small thorns and with leaves that are folded together in the bud. Besides, this plant has also been used to prevent soil erosion and to stabilize watersheds in semi-desert regions of Iran. In addition, the plant has been used as a healing agent from very early in the history to alleviate burn wounds, as well as to reduce gastrointestinal, respiratory and cough disorders, and to treat worm infection 9. In addition to applications in traditional medicine, in modern medicine, various properties of this plant including antioxidant, anti-bacterial and anti-fungal properties have been confirmed 10111213. Based on what has been discovered, this study aims to evaluate the antinociceptive and anti-inflammatory effects of A. eburnea extract in NMRI male mice.
Methods
Plant collection
Due to the abundance of A. eburnea in rural areas of Kerman district, shell roots were collected in this area in the Southeast of Iran, during April 2013. The plant materials were received at the Herbarium of Department of Pharmacognosy, School of Pharmacy, Kerman University of Medical Science, Iran
Preparation of the methanolic extract
Using the percolation method, approximately 100 g of dried plant material was extracted by using 80% methanol for 72 h at room temperature. To purify further, the crude extract was filtered through a filter paper. In the final step, the extract was concentrated in vacuum at 50°C by a rotary evaporator (Heidolph, Germany) and was kept at -20°C, until use 141516.
Animals
Groups of six male NMRI mice weighing from 25 to 30 gram with the same light-dark cycles (12:12-h) were used at the room temperature (21±1ºC). Enough food and water were provided for mice.
Ethics
The ethical approval required for this study was issued by the Ethics Committee of Kerman University of Medical Sciences, Kerman, Iran.
Antinociceptive effects
Tail-flick test
In the tail-flick test, an intense beam of light is focused on the middle one-third of animal's tail. In this experiment, five groups of six mice with 30 mice in total were treated with different doses of A. eburnea extract (250, 500, and 750 mg/kg) and were subjected to the tail-flick test to evaluate the terminal pain threshold. The light intensity of the tail flick apparatus (Sparco, Iran) was adjusted to make a 2 to 4 s latency time in the control animal. A 10-second cutoff time was chosen to prevent any possible tissue damage. Latency time was recorded three times with a 15-min interval for each set of the tail-flick test; the mean value of the latency time was considered as the thermal pain threshold (tail flick latency) 17.
Hot-plate test
The plate temperature of the device was set to 55±0.2 °C to evaluate pain sensitivity of the mice treated with different doses of A. eburnea extract (250, 500, and 750 mg/kg), normal saline, or morphine. The apparatus contained a plate with the diameter of 19 cm and a Plexiglas wall with the height of 30 cm (LE710 model, Lsi LETICA, Spain). The interval between the start of the experiment and the licking front paw or jumping was measured as the reaction time to thermal pain (maximum cutoff was considered 60s) 18.
Anti-inflammatory study
Xylene-induced ear edema
In this investigation, anti-inflammatory effects of were evaluated using the xylene-induced ear edema method which was described in earlier studies 17. Briefly, 30 mice were randomly divided into five groups (six mice in each group). One hour after the IP administration of the various doses of A. eburnea extract (250, 500, and 750 mg/kg), xylene was treated to the anterior surfaces of the right ear, and the left ear was used as a control. In this test, dexamethasone and normal saline were used as the positive and negative control respectively. In the next step, 120 min after the administration of xylene, mice were sacrificed and both ears were detached. 5-mm ear punch biopsies were collected and weighed. The difference between the weight of the left and the ear biopsies was considered as edema.
Rotarod test
In this study, we used the rotarod test to evaluate the motor coordination in tested animals. Before testing, mice were trained to stay for three min on a rolling rod (3 cm, diameter) rotating at 8 rpm. At the time of the test, three groups (six mice in each) were treated with different doses of A. eburnea extract (250, 500, and 750 mg/kg) and one group was treated with normal saline as the negative control. Finally, after the administration of A. eburnea extract and normal saline, mice were placed on the rolling rod, and the number of falls experienced by the mice during the procedure (three minutes) was recorded 1719.
Statistical analysis
The results of the experiments were analyzed by SPSS software version 17.0 (SPSS Inc., Chicago, IL, USA). To evaluate the difference between experimental groups, one-way ANOVA test was performed using Tukey's post-hoc test. At last, P<0.05 was considered statistically significant.
Results
The analgesic effect of A. eburnea extract on t ail flick test
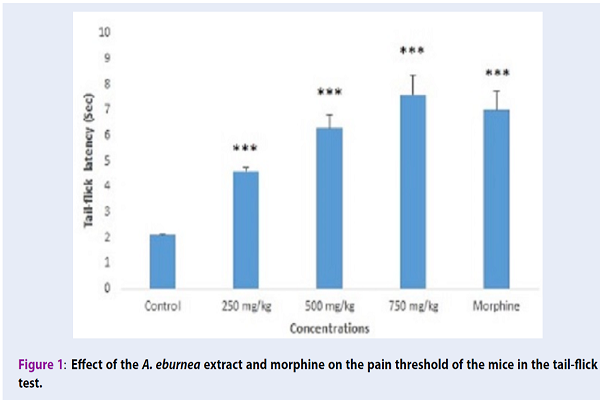
Figure 1 indicates the antinociceptive effects of A. eburnea extract in a dose-dependent manner in the tail-flick test. Groups treated with A. eburnea extract at the doses of 250, 500 and 750 mg/kg had a mean latency time of 4.6, 6.3 and 7.6 seconds, respectively; indicating a significant (p<0.05) antinociceptive effect compared to the control group. Although the time latency of the extract at the dose of 750 mg/kg was more than morphine, no significant difference was observed (p>0.05).
The analgesic effect of A. eburnea extract on hot-plate test
According to Figure 2, A. eburnea extract at the doses of 250, 500 and 750 mg/kg had a potent antinociceptive effect in a dose-dependent manner. The results showed a significant difference between the saline- and extract-treated groups (p<0.05). The reaction time of the extract-treated groups at the doses of 250, 500, and 750 mg/kg was 16.3, 21.6, and 26.6 seconds, respectively; Although the reaction time at the dose 750 mg/kg was more than that of morphine (24.3s), there was no significant difference between the two groups (p>0.05).
Effects of A. eburnea extract on xylene-induced ear edema in mice
Table 1 shows the findings obtained from the xylene-induced mice ear edema experiment.
The results showed that the administration of A. eburnea extract at the doses 250, 500 and 750 mg/kg significantly decreased the ear edema induced by xylene compared to the control group in tested mice (21.5, 50.9, and 69.6%, respectively). Whereas, dexamethasone at the dose of 10 mg/kg reduced the ear edema induced by xylene up to 66.9% in tested animals.
Rotarod test
In this study, the motor coordination after administration of the various doses of A. eburnea extract in tested animals was evaluated using the rotarod test. The obtained results showed that there is no significant (p>0.05) change in the sensory-motor test after the administration of A. eburnea extract at the doses of 250, 500 and 750 mg/kg.
| Group | Edema weight (mg) | % Inhibition |
| Control (normal saline) | 11.2 ±0.6 | |
| A. eburnea extract (250 mg/kg) | 8.8±1.15 | 21.5 |
| A. eburnea extract (500 mg/kg) | 5.5±0.51 | 50.9* |
| A. eburnea extract (750 mg/kg) | 3.4±0.5 | 69.6* |
| Dexamethsone (10 mg/kg) | 3.7±0.15 | 66.9 |
Discussion
Today, pain is considered one of the most widespread concerns with considerable social and economic impacts 3. Everyone may have experienced a variety of pains such as nociceptive, inflammatory, neuropathic, and functional pains which are caused by various neurobiological mechanisms. Although a number of analgesic medications are available to remedy a broad spectrum of pain and inflammation, such as non-steroidal anti-inflammatory drugs (NSAIDs), glucocorticoids and opioids 12, their adverse side effects and also ineffectiveness of some medications for particular conditions necessitate the constant investigation for new pain relievers.
Recent studies demonstrated that plants and their products are vital sources to find proper and less toxic reagents 720. In modern medicine, the ethnobotanical studies have revealed different medicinal possessions of herbal such as antinociceptive, anti-inflammatory, anti-cancer, and antimicrobial effects 21. To the best of our knowledge, a wide range of medicinal herbs such as Citrullus colocynthis, Curcuma longa, Crocus sativus, Elaeagnus angustifolia, Ginkgo biloba, Mitragyna speciosa, Momordica charantia, Nigella sativa, Ocimum sanctum, Phyllanthus amarus, Zataria multiflora, Crocus sativus, Zhumeria majdae, Elaeagnus angustifolia, Urtica pilulifera, and Rosa damascene are well-known as analgesic in modern medicine 22. Therefore, this study aims to evaluate the antinociceptive and anti-inflammatory effects of A. eburnea extract using the tail-flick and hot-plate tests in NMRI mice.
The obtained findings in the tail-flick and hot-plate tests demonstrated that A. eburnea extract at the doses of 250, 500 and 750 mg/kg had a potent antinociceptive effect in a dose-dependent manner. The results showed a significant difference the saline- and extract-treated groups (p<0.05). The reaction time of the extract-treated groups at the dose of 750 mg/kg was more than that of morphine, but there was no significant difference between them (p>0.05).
One of the main tests to evaluate the antinociceptive effects of tested agents is the hot-plate test 23. We found that the A. eburnea extract had a dose-dependent response in reducing heat-induced pain. Subsequently, the tail-flick test is applied to study the spinal responses and to detect the central analgesic route 24, this extract may induce its analgesic effect through the central nervous system. On the other hand, in the hot-plate test, A. eburnea extract demonstrated an analgesic effect based on a dose-dependent manner; so there was a significant difference between the extract-treated groups and saline-treated group (p<0.05). These results also showed that the antinociceptive effect in the extract-treated group at the dose of 750 mg/kg was more potent than that of morphine. However, this difference was not significant. These findings suggested that A. eburnea probably showed antinociceptive effects via the central opioid receptors or an increase in the release of endogenous opiopeptides 2324.
Regarding the anti-inflammatory effect of A. eburnea extract, we found that the administration of A. eburnea extract especially at the doses of 500 and 750 mg/kg significantly decreased the ear edema induced by xylene compared to the control group in tested mice. Regarding the antinociceptive and anti-inflammatory effects of plants in Rosaceae family, there are few studies, for example, Vongtau et al 2004 demonstrated the Parinari polyandra methanolic extract have considerable anti-inflammatory and anti-nociceptive effect particularly at the dose of 200 mg/kg in mice and rats 25. In the other study, Mahmoodi et al (2016) showed that Potentilla reptans extract at the doses of 50 and 100 mg/kg have remarkable analgesic effects compared to the control group 26. Based on the previous studies, in phytochemical screening of plants in Rosaceae family, the presence of flavonoids, tannins, and saponin glycoside have been proven 27. Since the antinociceptive and anti-inflammatory effects of these compounds have been shown 2829; a number of studies have shown that flavonoids and tannins components in the plants in Rosaceae family showed their antinociceptive effects through opioid receptors, nitric oxide pathway as well as via the inhibition of vanilloid receptors and the glutamatergic system 3031. Therefore, it is probably that the antinociceptive and anti-inflammatory effects of A. eburnea may be related to the presence of these compounds.
Conclusion
There are some limitations in this study such as there was no phytochemical analysis of A. eburnean extract, or no other analgesic and anti-inflammatory test such as formalin test was used. The results demonstrated that A. eburnea extract has potent antinociceptive and anti-inflammatory effects in mice. Nevertheless, the precise mechanisms responsible for these effects remain to be studied.
Competing Interests
No conflict of interest to declare.
Authors' Contributions
Nasrin Galehdar: Study design, writing
Mostafa Rezaeifar: Data collection and experiments.
Maryam Rezaeifar: Data analysis
Mehdi Rezaeifar: Supervisor, writing
Acknowledgments
The authors thank from the staff of Pharmaceutic Research Center, Kerman University of Medical Sciences, Kerman, Iran.
References
-
Lamont
L. A.,
Tranquilli
W. J.,
Grimm
K. A..
Physiology of pain. The Veterinary Clinics of North America. Small Animal Practice.
2000;
30
:
703-28
.
-
Kidd
B. L.,
Urban
L. A..
Mechanisms of inflammatory pain. British Journal of Anaesthesia.
2001;
87
:
3-11
.
-
Breivik
H.,
Collett
B.,
Ventafridda
V.,
Cohen
R.,
Gallacher
D..
Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. European Journal of Pain (London, England).
2006;
10
:
287-333
.
-
Stankov
S. V..
Definition of inflammation, causes of inflammation and possible anti-inflammatory strategies. The Open Inflammation Journal.
2012;
5
:
1-9
.
-
Sycha
T.,
Anzenhofer
S.,
Lehr
S.,
Schmetterer
L.,
Chizh
B.,
Eichler
H. G..
Rofecoxib attenuates both primary and secondary inflammatory hyperalgesia: a randomized, double blinded, placebo controlled crossover trial in the UV-B pain model. Pain.
2005;
113
:
316-22
.
-
Adedapo
A. A.,
Aremu
O. J.,
Oyagbemi
A. A..
Anti-oxidant, anti-inflammatory and antinociceptive properties of the acetone leaf extract of vernonia amygdalina in some laboratory animals. Advanced Pharmaceutical Bulletin.
2014;
4
:
591-8
.
-
Rocha
L. G.,
Almeida
J. R.,
Macêdo
R. O.,
Barbosa-Filho
J. M..
A review of natural products with antileishmanial activity. Phytomedicine.
2005;
12
:
514-35
.
-
Madani
B.,
Rahemi
M.,
Baninasab
B.,
Mahmoodi
M..
Morphological evaluation of three native species of Amygdalus in iran. Horticulture, Environment and Biotechnology.
2009;
50
:
63-7
.
-
Mozaffarian
V..
Trees and Shrubs of IranFarhang Moaser: Latin, Persian; 2005.
Google Scholar -
Rezaeifar
M,
Behfarnezhad
M,
Moradi
M,
Mehrabani
M,
Mahmoudvand
H.
Antibacterial effects of various extracts of Amygdalus eburnea on some most common bacteria in burning. Pharm Lett.
2016;
8
:
110-2
.
-
Rezaeifar
M.,
Rezaeifar
M..
Antioxidant properties of the methanolic extract of the shell root of Amygdalus eburnean. International Journal of Pharm Tech Research.
2016;
9
:
514-8
.
-
Rezaeifar
M.,
Rezaeifar
M..
In vitro antidermatophytic effects of the methanolic extract of the Amygdalus eburnean. International Journal of Pharm Tech Research.
2016;
9
:
509-12
.
-
Rezaeifar
R.,
Mousavi
S. A.,
Mehrabani
M.,
Sepahvand
A..
Evaluation of the antifungal effects of various extracts of Amygdalus eburnean on some fungal pathogens. Der Pharma Chemica.
2016;
8
:
140-2
.
-
Mahmoudvand
H.,
Asadi
A.,
Harandi
M. F.,
Sharififar
F.,
Jahanbakhsh
S.,
Dezaki
E. S..
In vitro lethal effects of various extracts of Nigella sativa seed on hydatid cyst protoscoleces. Iranian Journal of Basic Medical Sciences..
2014;
17
:
1001-6
.
-
Tavakoli Kareshk
A.,
Keyhani
A.,
Mahmoudvand
H.,
Tavakoli Oliaei
R.,
Asadi
A.,
Andishmand
M..
Efficacy of the Bunium persicum (Boiss) essential oil against acute toxoplasmosis in mice model. Iranian Journal of Parasitology.
2015;
10
:
625-31
.
-
Saedi Dezaki
E.,
Mahmoudvand
H.,
Sharififar
F.,
Fallahi
S.,
Monzote
L.,
Ezatkhah
F..
Chemical composition along with anti-leishmanial and cytotoxic activity of Zataria multiflora. Pharmaceutical Biology.
2016;
54
:
752-8
.
-
Hosseinzadeh
H.,
Haddadkhodaparast
M. H.,
Arash
A. R..
Antinociceptive, antiinflammatory and acute toxicity effects of Salvia leriifolia Benth seed extract in mice and rats. Phytother Res.
2003;
17
:
422-5
.
-
Mahmoudvand
H.,
Ziaali
N.,
Ghazvini
H.,
Shojaee
S.,
Keshavarz
H.,
Esmaeilpour
K..
Toxoplasma gondii infection promotes neuroinflammation through cytokine networks and induced hyperalgesia in BALB/c mice. Inflammation.
2016;
39
:
405-12
.
-
Hosseinzadeh
H.,
Khoshdel
M.,
Ghorbani
M..
Antinociceptive, anti-inflammatory effects and acute toxicity of aqueous and ethanolic extracts of Myrtus communis L. Aerial parts in mice. Journal of Acupuncture and Meridian Studies.
2011;
4
:
242-7
.
-
Mahmoudvand
H.,
Sharififar
F.,
Rahmat
M. S.,
Tavakoli
R.,
Dezaki
E. S.,
Jahanbakhsh
S..
Evaluation of antileishmanial activity and cytotoxicity of the extracts of Berberis vulgaris and Nigella sativa against Leishmania tropica. Journal of Vector Borne Diseases.
2014;
51
:
294-9
.
-
Sheng-Ji
P..
Ethnobotanical approaches of traditional medicine studies: some experiences from Asia. Pharmaceutical Biology.
2001;
39
:
74-9
.
-
Forouzanfar
F.,
Hosseinzadeh
H..
Medicinal herbs in the treatment of neuropathic pain: a review. Iranian Journal of Basic Medical Sciences..
2018;
21
:
347-58
.
-
Hosseinzadeh
H.,
Ramezani
M.,
Salmani
G..
Antinociceptive, anti-inflammatory and acute toxicity effects of Zataria multiflora Boiss extracts in mice and rats. Journal of Ethnopharmacology.
2000;
73
:
379-85
.
-
Hosseinzadeh
H.,
Behravan
E.,
M Soleimani
M.,
Arash
A. R..
Antinociceptive, antiinflammatory Pistacia vera extract in mice and rats. Iranian Journal of Pharmaceutical Research.
2011;
10
:
821-8
.
-
Vongtau
H. O.,
Abbah
J.,
Ngazal
I. E.,
Kunle
O. F.,
Chindo
B. A.,
Otsapa
P. B..
Anti-nociceptive and anti-inflammatory activities of the methanolic extract of Parinari polyandra stem bark in rats and mice. Journal of Ethnopharmacology.
2004;
90
:
115-21
.
-
Mahmoodi
M,
Mohammadi
S,
Enayati
F.
Evaluation of the antinociceptive effect of hydroalcoholic extract of Potentilla reptans L. in the adult male rat. SSU_Journals.
2016;
24
:
201-210
.
-
Potter
D..
Phylogeny and classification of Rosaceae. Plant Systematics abd. Evaluation.
2007;
266
:
5-43
.
-
de Barros Viana
G. S.,
Bandeira
M. A.,
Moura
L. C.,
Ribeiro
R..
Analgesic and Antiinflammatory Effects of the Tannin Fraction from Myracrodruon urundeuva Fr. All. Phytotherapy Research.
1997;
11
:
118-22
.
-
Qnais
E.,
Abu-Safieh
K.,
Abu-Dieyeh
M. A.,
Abdulla
F. A..
Antinociceptive Effect of Two Flavonoids from Aloysia Triphylla L. Jordan Journal of Biological Sciences.
2009;
4
:
167-70
.
-
Afify
E. A.,
Alkreathy
H. M.,
Ali
A. S.,
Alfaifi
H. A.,
Khan
L. M..
Characterization of the Antinociceptive Mechanisms of Khat Extract (Catha edulis) in Mice. Frontiers in Neurology.
2017;
8
:
69
.
-
Jaios
Erman Shah,
Rahman
Suzana Abdul,
Ching
Siew Mooi,
Kadir
Arifah Abdul,
Desa
Mohd Nasir Mohd,
Zakaria
Zainul Amirudin.
Possible mechanisms of antinociception of methanol extract of Melastoma malabathricum leaves. Revista Brasileira de Farmacognosia.
2016;
26
:
586-594
.
Comments
Downloads
Article Details
Volume & Issue : Vol 5 No 10 (2018)
Page No.: 2746-2751
Published on: 2018-10-23
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 4209 times
- Download PDF downloaded - 1267 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress



