Abstract
Objectives: This study was designed to characterize 12-lead electrocardiogram (ECG) for localization of the left free wall lateral accessory pathway (AP) in patients with typical Wolff-Parkinson-White (WPW) syndrome, to develop a new algorithm ECG for localizing APs, and to test the accuracy of the algorithm prospectively.
Method: We studied 129 patients; 84 patients had typical WPW syndrome with single anterograde AP identified by successful radiofrequency catheter ablation (RFCA), and were enrolled to build a new ECG algorithm for localizing left free wall APs. Then, the algorithm was tested prospectively in 45 patients and compared with the location of APs successfully ablated by RFCA.
Results: We found that the 12-lead ECG parameters in typical WPW syndrome, such as delta wave polarity in V1, R/S ratio in V1, transition of the QRS complex, and delta wave polarity in inferior, lead to diagnosis and localization of APs, with highest accuracy predicted from 74.5%-100%, and for development of a new ECG algorithm. From the 45 patients who were prospectively evaluated by the newly derived algorithm for the left free wall pathways, the sensitivity and specificity was high (from 75-100%).
Conclusion: The 12-lead ECG parameters in typical WPW syndrome are closely related to left free wall AP localization and can be used to develop a new ECG algorithm by the parameters above. Moreover, the new ECG algorithm can predict the location of APs with high accuracy.
Introduction
Wolff-Parkinson-White syndrome (WPW) is a form of ventricular preexcitation in which part of the ventricular myocardium is depolarized early by one or more accessory pathways (APs) that bypass the atrioventricular (AV) node, establishing a direct link between the atrium and the ventricle (called Kent Bundle). The 12-lead electrocardiogram (ECG) is characterized by a shortened PR, prolonged QRS, and Delta wave 12. Arrhythmias are frequent in WPW syndrome patients due to paroxysmal supraventricular tachycardia (PSVT), atrial fibrillation (AF), etc.; the most dangerous are ventricular fibrillation and sudden death 21.
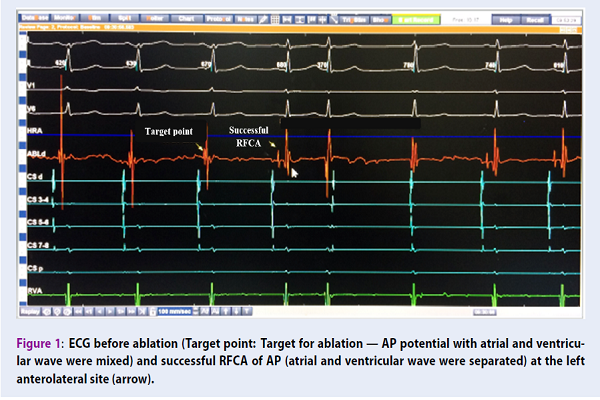
Nowadays, radiofrequency catheter ablation (RFCA) of APs requires precise localization of the AP along the mitral and tricuspid annulus (gold standard) 2. The 12-lead ECG is the first step for localization of AP in patients with WPW syndrome, up to now. The data obtained from the ECG parameters can be helpful in planning and shortening the RFCA procedure and fluoroscopy time 2.
According to many studies, the ratio of left free wall (the side of the mitral valve circle, except the septal location) is very common among APs. Localizing APs includes the left free wall and includes left anterolateral (LAL), left lateral (LL), and left posterolateral (LPL) pathways that can help quickly locate and approach an AP location- to facilitate mapping and to shorten time of radiofrequency ablation 13456.
Some published ECG algorithms have been based on predicting locations of left free wall APs 12457. However, many studies have shown that it is difficult to compare differences between other locations on the side of the mitral valve circle 457. Therefore, the purpose of this study was to analyze the 12-lead ECG for septal AP localization and successful RFCA to develop new ECG algorithms using simple parameters, as well as testing the algorithm to predict AP location.
Methods
Study design
The study was observational, cross-sectional, retrospective and prospective. We selected specificity as the standard for the study.
Patient inclusion and exclusion criteria
Patient inclusion criteria
The patients included in the study must have typical WPW syndrome and have a single anterograde AP which was successfully identified by RFCA.
Patient exclusion criteria
The patients excluded from the study must have had one of the following criteria: not treated with RFCA, not having enough information during their treatment, not agreeing to participate in the study, not having successful RFCA, or having more than one AP.
Study contents
We studied 129 patients with typical WPW syndrome who had a single AP in the left free wall location (along the free wall side of the mitral valve annulus), from January 2001 to May 2017, at Vietnam National Heart Institute, Bachmai Hospital. There are two phases of the study:
+ Phase 1: 84 patients with typical WPW syndrome who had a single anterograde left free wall AP identified by successful RFCA were enrolled to build a new ECG algorithm for localizing left free wall APs using simple parameters, from January 2001 to June 2016.
+ Phase 2: Next, the algorithm was tested prospectively in 45 patients to compare with the location of left free wall AP successfully ablated by RFCA, from June 2016 to May 2017.
WPW syndrome was defined by the 12-lead ECG, characterized by a shortened PR interval < 120 milliseconds, prolonged QRS duration ≥ 110 milliseconds, and with a delta wave. Secondary ST and T wave changes were directed opposite to the major Delta wave and QRS vector 1. Localization of APs was identified by successfully ablation by RCFA (gold standard) 2.
The annulus position of left free wall AP has 3 regions: left anterolateral (LAL), left lateral (LL), and left posterolateral (LPL). RFCA for APs is conducted through the ablating action of the catheter tip at the intersection of the AP and mitral valve or tricuspid valve. Localization of APs is confirmed by the catheter position for successful RFCA of each location (gold standard) 2.
The medical treatment was conducted per the procedure in the catheterization laboratory at Vietnam National Heat Institute, Bachmai General Hospital, Hanoi, Vietnam. We perform a full spectrum of cardiac and vascular interventions using the Phillips Advanced Allura Xper FD20 X-ray Biplane System (Phillips, Holland), a programmed cardiac stimulator instrument (integrated in the cardiac stimulator EP-4 System), Cardiac Stimulator EP-4 System, Radio Ampere Generator instrument, diagnostic EP catheter, and mapping and ablation catheter (St. Jude, USA).
Statistical Analysis
We set the AP location (confirmed by successful RFCA) as the dependent variable and the 12-lead ECG parameters as the independent variables. P-values < 0.05 were considered statistically significant. We calculated values of sensitivity (Se), specificity (Sp), positive predictive value (PPV), and negative predictive value (NPV) for the predicted AP location. The SPSS v. 21.0 software (IBM, USA) was used for analyzing the data.
Research ethics
The research proposal, database, medical records, and results were approved by the Committee of Science of Vietnam University of Military Medicine. The RFCA used in the research has been demonstrated to be highly effective and safe. The indications and safety of the medical treatment were approved by the Ethics Committee of Bachmai Hospital. The patients were explained about the procedure and provided signed consent for catheter ablation. All patients’ medical records were kept confidential and used for research purposes only.
Results
The study population consisted of 129 patients: 71 men (55%) and 58 women (45%), with age of 45.1 ± 14.6 years (range from 19 to 79 years of age).
Characteristics of 12-lead ECG for localization of septal AP
The study population consisted of 84 patients (Group I): 40 men (52.4%) and 40 women (47.6%), with age of 44.9 ± 14.5 years (range from 19 to 79 years of age). Left free wall APs were found in 84 patients: 55 patients had left lateral (65.5%), 17 patients had left anterolateral (20.2%), and 12 patients had left posterolateral (14.3%).
Transition characteristics of the QRS complex on 12-lead ECG with left free wall location
Classified transition of left free wall location was most common at after V1,V2 lead (V3-V6) or before V1 lead; this was found in 72 patients (i.e. 85.7% of the total number of 84 left free wall pathways).
Characterization of delta wave polarity in V1 lead with left free wall lateral location
Left free wall pathways had positive delta wave that was most common at V1 lead; this was found in 83/84 patients (98.9%).
Characterization of delta wave polarity in at least 2/3 inferior lead with left anterolateral or left posterolateral free wall pathway
Left anterolateral pathways had positive delta wave that were most common in at least 2/3 inferior lead (DII, DIII, AVF); this was found in 17/17 patients (100%). Meanwhile, left posterolateral pathways had negative delta waves that were most common in at least 2/3 inferior leads; this was found in 11/12 patients (91.7%). However, left lateral pathways had positive delta waves that were most common in at least 2/3 inferior leads; this was found in 52/55 patients (94.5%).
Therefore, the group with “left anterolateral and left lateral pathways” had positive delta waves that were most common in at least 2/3 inferior lead found in 69/72 patients (95.8%), and left posterolateral pathways had negative delta wave most common in at least 2/3 inferior lead as above (91.7%).
For classified R/S ratio of V1 lead for the left anterolateral and left lateral pathway, the anterolateral was most common with R/S > 1 at V1 lead; this was found in 13 patients contributing to 76.5% among a total number of 17 patients. The left lateral was most common with R/S < 1 (62.3%) or QRS complex’R morphology at V1 lead; this was found in 41 patients contributing to 74.5% among a total number of 55 patients with left lateral pathways. Moreover, left lateral had R/S > 1 at V1 lead in 14/55 patients (25.5%) Table 1.
| CharacterizationLeft free wall | (+/-) Delta inV1 lead | (+/-) Delta in at least 2/3 inferior lead | R/S in V1 |
| Left anterolateral | ( + ) | ( + ) | R/S > 1 |
| Left lateral | ( + ) | ( + ) | R/S <1 or QRS: R |
| Left posterolateral | ( + ) | ( - ) |
Accuracy of the new ECG algorithm for localizing APs
The study population consisted of 45 patients (Group II): 27 men (60%) and 18 women (40%), with age of 45.6 ± 15.0 years (range from 19 to 70 years of age).
Left free wall pathways were found in 45 patients, with 25/45 patients having left lateral (54.3%), 12/45 patients having left anterolateral (26.7%), and 8/45 patients having left posterolateral (17.8%) pathways.
Localization of free wall lateral AP by transition characteristics of the QRS complex on 12-lead ECG
The accuracy of the algorithm for localizing APs in left free wall location by QRS complex transition was most common at/after V1,V2 lead (V3-V6) or before V1 lead; this was found in 44 patients, contributing to 97.8% among the total number of 45 left free wall pathways (sensitivity was 97.8%).
Localization of left AP pathways by delta wave polarity in V1 lead
The accuracy of the algorithm for localizing APs in free wall pathways belongs to the left side location by positive delta wave, which was most common at the V1 lead; this was found in 44/45 patients (97.8%), giving a sensitivity of 97.8%.
Localization of other positions in the left free wall APs by positive or negative delta waves in at least 2/3 inferior leads
| Location (+/-) Delta wave in inferior lead | Left antero-lateral (n) | Left lateral (n) | Left postero- lateral (n) | Total |
| Positive delta wave in at least 2/3 inferior | 12 | 25 | 2 | 39 |
| Negative delta wave in at least 2/3 inferior | 0 | 0 | 6 | 6 |
| Total (n) | 12 | 25 | 8 | 45 |
The accuracy of the algorithm for localizing APs in left anterolateral and left lateral by positive delta wave in at least 2/3 inferior lead (DII, DIII, AVF) were 12/12 (100%) and 25/25 (100%), respectively. Therefore, the accuracy of the algorithm for localizing APs in the group of “left anterolateral and left lateral pathway” or “left posterolateral pathway”, by positive delta wave or negative delta waves, in at least 2/3 inferior lead was very significantly high, giving a sensitivity of 100%, specificity of 75%, PPV of 94.9% and NPV of 100%.
Localization of left anterolateral or left lateral pathways by the R/S ratio at V1 lead
| Location R/S ratio at V1 | Left antero lateral | Left lateral | Total | ||
| Rate (%) | Rate (%) | ||||
| R/S > 1 | 11 | 91,7% | 6 | 24% | 17 |
| R/S < 1 | 0 | 0% | 10 | 40% | 10 |
| QRS morphology: R pattern | 1 | 8,3% | 9 | 36% | 10 |
| Total (n) | 12 | 25 | 37 |
The accuracy of the algorithm for localizing APs was evaluated in the left anterolateral or left lateral position by R/S ratio > 1 (91.7%) or R/S ratio < 1 (40%), and by QRS complex morphology’s R pattern (36%) at V1 lead. Therefore, the accuracy of the two position was significantly higher, giving a sensitivity of 91.7%, specificity of 76%, PPV of 64.7%, and NPV of 95%. Overall, the accuracy of the new ECG algorithm for localizing APs sites showed high accuracy (Table 2Table 3Table 4).
| Left free wall accessory pathways (n = 45) | Se (%) | Sp (%) | PPV (%) | NPV (%) |
| Sensitivity for accuracy for the free wall lateral APs | 97.8% | |||
| Left side APs (left free lateral APs) | 97.8% | |||
| Group of “left anterolateral and left lateral” with “left posterolateral” APs | 100% | 75% | 94.9% | 100% |
| Left anterolateral or left lateral by R/S ratio at V1 lead | 91.7% | 76% | 64.7% | 95% |
Patients (n = 45) with left free wall AP required less procedure time (ablation time was 42.4 ± 12.8 min) and less fluoroscopy time (7.2 ± 3.4 min).
DISCUSSION
Characterization
Transition characteristics of the QRS complex on 12-lead ECG with left free wall location
Classified transition of left free wall location was most common at before V1 lead (Figure 4A,C,D) or after V1V2 lead (Figure 4B), as noted (85.7%). This is a characteristic that can be different between free wall and septal location. Some studies have shown that transition of QRS complex can be used for predicting locations of septal or free wall AP but these studies have only focused on differences between right free wall and right septal location. Most studies have not yet found differences between left free wall and left septal location 134. Thus, we can predict that the left free wall belongs to free wall location by QRS transition at before V1 or after V1V2 lead.
Characterization of delta wave polarity in V1 lead with left free wall
Left free wall had positive delta wave that was most common at V1 lead (100%) (Figure 4). This is very useful in selecting the approach of the catheter- vein or artery. Left-side AP were ablated with retrograde arterial approach (while right-sided AP were ablated with the use of transvenous atrial approach through the femoral vein) 2.
Some ECG algorithms have been published that can predict locations of left-sided or right-sided APs by positive/negative delta wave 12. Moreover, other studies showed the diagnosis of left or right-sided APs by other ECG parameters; D’Avila A. et al. (1995) showed that positive or negative QRS complex in V1 can be used in diagnosis of left or right-sided AP 3. Chiang C.E. et al. (1995) showed that an R/S ratio >1 suggested a left-sided AP 4. Arruda M.S. et al. (1998) also found that R/S >1 in V1 lead corresponded to the left free location and R/S <1 in V1 lead corresponded to the right side 5. Dar M.A. et al. (2008) also used an R/S ratio <1 in a VL lead to predict left side 6. Taguchi N. et al. (2014) used R/S ratio < 0.5 or R/S > 0.5 in V1 lead to predict right or left-sided APs 7. We had not known that R/S ratio at a VL lead as well as R/S ratio (or QRS) in V1 lead could suggest a left free wall pathway.
Characterization of delta wave polarity in at least 2/3 inferior lead (DII, DIII, AVF) with left anterolateral or left posterolateral pathway
A characteristic electrocardiogram of a patient with left anterolateral pathway showed strongly positive delta waves in at least 2/3 inferior leads (II, III, aVF), as noted (100%) (Figure 4A), while the left posterolateral pathway group had strongly negative delta waves in at least 2/3 inferior leads (II, III, aVF), as noted (91.7%) (Figure 4D). Specialized, left lateral pathway had positive delta wave that were most common at least 2/3 inferior leads, a noted (94.5%) (Figure 4B,C) as the same characteristic left anterolateral pathway (Figure 4A). Therefore, one can build a group that includes “left anterolateral and left lateral pathways”, in which the positive delta wave was most common at least in 2/3 inferior lead, as noted (95.8%), and “left posterolateral pathways” had negative delta waves that were most common at least 2/3 inferior lead, as above (91.7%).
According to the statistics as above, the left anterolateral and left lateral pathways are often found in the positive delta location in at least 2/3 inferior lead. We evaluated the characteristic R/S ratio at V1 lead in these two regions. The result showed that the left anterolateral position was most common with R/S ratio >1 at V1 lead (76.5%), while the left lateral was most common with R/S < 1 (Figure 4B) or QRS complex’s R morphology (Figure 4C) at V1 lead (74.5%). Thus, these parameters (R/S) help to suggest that left antero lateral or left lateral pathways exist but not at high accuracy. This can be explained by the fact that between two location there are plenty of sequential zones that are similar in electrophysiological angle; thus, there can be many similarities.
Many studies have show the difficulty in localizing between left anterolateral or left lateral pathways, as well as difficulty in discerning differences between other positions of the left free wall pathways. Taguchi N. et al. (2014) selected two locations with “LA & LL pathways” and “LP & LPL pathways” 7. Iturralde T.P. et al. (1996) selected two locations for left free wall that included “LPL & LAS pathways” and “LIP & LI pathways” 8.
Thus, we suggest that “LA & LL pathways” and “LPL pathway’’ are represented by positive or negative delta wave in at least 2/3 inferior, different between LA and LL position by R/S ratio > 1 or R/S < 1, and R in V1 lead (Table 1 Figure 3). This can help the doctors to perform a rapid onset of AP location on the mitral valve forwards or backwards, or within 1-2 cm of the valve, and can help to facilitate mapping techniques and shorten time radiofrequency ablation 12.
Accuracy of new ECG algorithm for localizing left free wall AP
We have developed a new algorithm using some simple ECG parameters in the left free wall belong to left side pathways, represented by positive delta wave at V1 lead, left free wall site APs by QRS complex transition at before V1 lead or after V1V2 lead. “Left anterolateral and left lateral” group or left posterolateral sites of Aps showed positive/negative delta waves in at least 2/3 inferior; left anterolateral and left lateral had R/S > 1 or R/S < 1, R.
The algorithm was then tested prospectively in 45 patients and compared with the location of APs in successful ablation by RF. The sensitivity, specificity, positive predictive value and negative predictive value of the diagnosed algorithm for AP sites were then calculated to high accuracy (Table 4).
Localization of free wall lateral location (AP group) by transition characteristics of the QRS complex on 12-lead ECG
Accuracy of the algorithm for localizing APs in left free wall location by QRS complex transition was at after V1,V2 lead (V3-V6) or before V1 lead, with very high sensitivity of 97.8%.
Accordingly, Dar M.A. et al. (2008) showed that the septal or lateral APs occurred at and by the QRS complex transition at V1V2 or after V1V2 (lead with Se of 97% and Sp of 95%) 6.
Localization of left AP pathways by delta wave polarity in V1 lead
The accuracy of the algorithm for localizing APs in left free wall pathways belong to left location by positive delta wave most common at V1 lead with very high accuracy. Given a sensitivity of 97.8%, Chang C.E. et al. (1995) showed the left side or right side pathways by positive/negative delta wave at V1 lead with Se of 94.4% and Sp of 87.5% 4.
Localization of other position of left free wall pathways
Localization of other positions of left free wall pathways by positive delta wave or negative delta wave in at least 2/3 inferior lead
Accuracy of the algorithm for localizing APs in group of “includes left anterolateral and left lateral pathways” or “left posterolateral pathways” by positive/negative delta wave in at least 2/3 inferior lead was very significantly higher, giving a sensitivity of 100%, specificity of 75%, PPV of 94.9% and NPV of 100% (Table 2). Dar M.A. et al. (2008) showed that the antero or postero APs by positive/negative delta waves in common at inferior lead had Se and Sp been from 85-100% 6.
Localization of left anterolateral or left lateral pathways by the R/S ratio at V1 lead
Accuracy of the algorithm for localizing APs in the left anterolateral or left lateral position by R/S ratio > 1 or R/S < 1, R. However, R/S has been significantly high, giving a sensitivity of 91.7%, specificity of 76%, PPV of 64.7% and NPV of 95% (Table 3). However, the predictive value was not high (64.7%); Therefore, the doctor must be attention to consideration of these cases during procedure of the mapping and radiofrequency ablation.
| Authors | Accessory athway Location | Mean ProcedureTime (minute) | Mean Fluoroscopy Time (minute) |
| Lemery R. et al . (1992) 9 | Left free wall (n = 36) | 162.0 ± 48.0 | 46.0 ± 24.0 |
| Dong T.V. (2006) 10 | Left lateral AP (n=47) | 82.9 ± 33.0 | 18.5 ± 10.7 |
| Left posterolateral (n=27) | 82.4 ± 51.6 | 19.9 ± 13.2 | |
| Left anterolateral (n=21) | 92.8 ± 42.7 | 23.3 ± 9.5 | |
| Schwagten B. et al. (2010) 11 | Left side AP (n = 10) | 87.1 ± 30.8 | 14.4 ± 4.7 |
| Our research (2016-2017) | Left free wall (n = 45) | 42.4 ± 12.8 | 7.2 ± 3.4 |
The potential to predict a successful ablation site can help decrease fluoroscopy time and significantly shorten procedure time (Table 5). By fluoroscopy safety guidelines, according to Singer (1993), mean fluoroscopy time per case > 48 min, and > 4 cases per week, can cause chromosomal aberration 12.
Conclusions
From our study in 129 patients, we have developed a new algorithm for localizing AP for the left free wall using 84 patients with typical WPW syndrome, and validated it. We found that the left free wall had positive delta wave that was most common at V1 lead (98.9%), and QRS complex transition was most common at after V1V2 lead or before V1 lead (85.7%). Anterolateral as well as left lateral pathways had positive delta waves that were most common in at least 2/3 inferior lead (100%) and posterolateral pathways had negative delta wave that was most common in at least 2/3 inferior lead (91.7%); they were different in LAL and LL region by R/S > 1 and R/S < 1 or R.
This algorithm was tested prospectively in 45 patients and compared with the location of APs determined by successful ablation by RFCA. The new algorithm was demonstrated to have high accuracy as well as sensitivity (from 75% to 100%), and could facilitate radiofrequency ablation in patients with left side AP as well as left free wall pathways. The potential to predict AP location is very important in affecting fluoroscopy time and procedure time (by significantly shortening them), when using the parameters as above for the prediction criteria of the left free wall location.
Competing Interests
The authors declare that there is no conflict of interest regarding the publication of this article.
Authors' Contributions
Si CD: designed the study, collected data, conducted the statistical analysis and wrote the manuscript.
Khanh PQ and Dong TV: are revised the manuscript during the review process.
Acknowledgements
Vietnam University of Military Medicine & Vietnam National Heart Institute, Bachmai Hospital.
Abbreviations
AP: Accessory pathway
APs: Accessory pathways
AV node: Atrioventricular node
AV: Atrioventricular
ECG: Electrocardiogram
RFCA: Radiofrequency catheter ablation
WPW: Wolff-Parkinson-White
References
-
Schwagten
B.,
Jordaens
L.,
Rivero-Ayerza
M.,
Belle
Y. Van,
Knops
P.,
Thornton
I. A..
A randomized comparison of transseptal and transaortic approaches for magnetically guided ablation of left-sided accessory pathways. Pacing and Clinical Electrophysiology.
2010;
33
:
1298-303
.
View Article PubMed Google Scholar -
T.V. Dong.
Doctor of Philosophy Thesis in Medicine: Research in Electrophysiology and treatment of Wolff-Parkinson-White Syndrome by Radiofrequency Catheter Ablation. Doctor of Philosophy.
2006
.
-
Lemery
R.,
Talajic
M.,
Roy
D.,
Coutu
B.,
Lavoie
L.,
Lavallée
E..
Success, safety, and late electrophysiological outcome of low-energy direct-current ablation in patients with the Wolff-Parkinson-White syndrome. Circulation.
1992;
85
:
957-62
.
View Article PubMed Google Scholar -
Surawicz
B.,
Knilans
T. K.,
Chou
T. C..
2008.
Google Scholar -
Basiouny
T..
Prospective Validation of A Sezer ECG Algorithm For Localization of Accrssory Pathways in Patients With Wolff-Parkinson-White Syndrome. Al-Azhar Assiut Medical Journal.
2012;
10
:
127-53
.
-
d’Avila
A.,
Brugada
J.,
Skeberis
V.,
Andries
E.,
Sosa
E.,
Brugada
P..
A fast and reliable algorithm to localize accessory pathways based on the polarity of the QRS complex on the surface ECG during sinus rhythm. Pacing and Clinical Electrophysiology.
1995;
18
:
1615-27
.
View Article Google Scholar -
Chiang
Chern-En,
Chen
Shih-Ann,
Teo
Wee Siong,
Tsai
Der-Shang,
Wu
Tsu-Juey,
Cheng
Chen-Chuan,
Chiou
Chuen-Wang,
Tai
Ching-Tai,
Lee
Shih-Huang,
Chen
Chung-Yin.
An accurate stepwise electrocardiographic algorithm for localization of accessory pathways in patients with Wolff-Parkinson-White syndrome from a comprehensive analysis of delta waves and R/S ratio during sinus rhythm. The American journal of cardiology.
1995;
76
:
40-46
.
-
Arruda
M. S.,
McClelland
J. H.,
Wang
X.,
Beckman
K. J.,
Widman
L. E.,
Gonzalez
M. D..
Development and validation of an ECG algorithm for identifying accessory pathway ablation site in Wolff-Parkinson-White syndrome. Journal of Cardiovascular Electrophysiology.
1998;
9
:
2-12
.
View Article PubMed Google Scholar -
Dar
M Ashraf,
SHEIKH
SHABBIR HUSSAIN,
ABID
ABDUL REHMAN,
MALLICK
NADEEM HAYAT.
Localization of Accessory Pathways According to AP Fitzpatrick Ecg Criteria in Patents with Wolff-Parkinson-White Syndrome in Our Population. Pakistan Heart Journal.
2012;
41
.
-
Taguchi
N.,
Yoshida
N.,
Inden
Y.,
Yamamoto
T.,
Miyata
S.,
Fujita
M..
A simple algorithm for localizing accessory pathways in patients with Wolff-Parkinson-White syndrome using only the R/S ratio. Journal of Arrhythmia.
2014;
30
:
439-43
.
View Article Google Scholar -
Iturralde
P.,
Araya-Gomez
V.,
Colin
L.,
Kershenovich
S.,
Micheli
A. de,
Gonzalez-Hermosillo
J. A..
A new ECG algorithm for the localization of accessory pathways using only the polarity of the QRS complex. Journal of Electrocardiology.
1996;
29
:
289-99
.
View Article PubMed Google Scholar -
Singger
I..
Clinical manual of electrophysiologyWilliams & Wikins: Baltimore; 1993.
Google Scholar
Comments
Downloads
Article Details
Volume & Issue : Vol 5 No 11 (2018)
Page No.: 2832-2840
Published on: 2018-11-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 6962 times
- Download PDF downloaded - 1272 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress





