Abstract
Cardiac disease is the second common cause of syncope in emergency departments. Patients with Cardiac syncope have a higher risk of mortality than those who have a non-cardiac problem. Brain natriuretic peptide (BNP) as a cardiac marker has not thoroughly been evaluated in patients with syncope. This article focuses on the studies that have assessed BNP and NT-pro-BNP in cardiac and non-cardiac syncope patients in emergency departments.
Introduction
Syncope is defined as a temporary loss of consciousness followed by spontaneous and complete recovery 1. In general populations, syncope is a common problem with the lifetime prevalence of 42% 2. It is estimated that 3% of referrals to emergency departments and 2% of inpatient admissions are due to syncope, and 6 out of 1000 people are affected by this problem every year 34. Kapoor et al. published one of the first prospective syncope studies and showed that the risk of mortality due to syncope in a 12-month follow-up was 14% 5. Serious underlying conditions such as dysrhythmia, structural heart disease, and significant hemorrhage can be the causes of syncope which ultimately lead to mortality and morbidity. The underlying conditions can be cardiac or vascular. The cardiac conditions are dysrhythmia and myocardial infarction (MI), and the vascular conditions are hemorrhage, aortic dissection, and pulmonary embolism 67. The serum marker BNP which is increasingly established in emergency departments for the diagnosis of acute heart failure can reflect the presence of structural heart disease 8910. Many studies have stated that cardiac syncope is caused by reduced cardiac output that is associated with impaired hemodynamic in arrhythmia or structural cardiac disorders 11. Therefore, brain natriuretic peptides are candidates for diagnosis of cardiac syncope. During the last decade, few studies were conducted to assess the role of BNP in isolating cardiac from non-cardiac syncope. This paper aimed to discuss the studies that evaluated the effect of brain natriuretic peptides on diagnosis and prediction of cardiac syncope in emergency departments.
Syncope Risk Stratification in Emergency Departments
In risk stratification and diagnosis of syncope, we must consider three major issues addressed by Costantino et al. 12:
Differentiating patients with syncope from those with loss of consciousness of no syncopal source
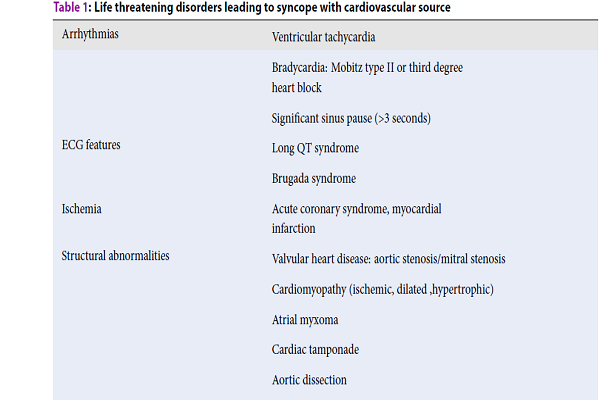
According to the European Society of Cardiology (ESC) guidelines, syncope is defined as a transient loss of consciousness (T-LoC) caused by transient cerebral hypo-perfusion characterized by loss of consciousness followed by spontaneous and complete recovery 13. Therefore, syncope must be distinguished from T-LoC not induced by cerebral hypoperfusion Table 1.
Distinguishing patients with syncope from those who have fallen
Most of the time, distinguishing syncope from fall in clinical practice is impossible and exhausting. Taking a careful history from a witness plays a crucial role in facilitating the diagnosis during the early evaluation in the ED.
Determining how to manage patients presenting to the ED with near syncope or pre-syncope
Management of the pre-syncope and near syncope patients is largely heterogeneous worldwide at present 1114. As Costantino et al. mentioned, pre-syncope or near syncope refers to the feeling of impending LoC without losing consciousness. Several symptoms and physical signs contribute to this feeling, such as weakness, tunnel vision, dizziness, nausea, sweating, and pallor.
Many studies performed in emergency departments exclude presyncope or near syncope because it is often assumed that these patients have a good prognosis. However, Grossman et al. compared the clinical outcomes of the patients with pre-syncope and the individuals with syncope, and no statistically significant difference was found between the two groups. They concluded that the prognosis of near syncope was similar to that of syncope.
| Arrhythmias | Ventricular tachycardia |
| Bradycardia: Mobitz type II or third degreeheart block | |
| Significant sinus pause (>3 seconds) | |
| ECG features | Long QT syndrome |
| Brugada syndrome | |
| Ischemia | Acute coronary syndrome, myocardialinfarction |
| Structural abnormalities | Valvular heart disease: aortic stenosis/mitral stenosis |
| Cardiomyopathy (ischemic, dilated ,hypertrophic) | |
| Atrial myxoma | |
| Cardiac tamponade | |
| Aortic dissection | |
| Significant hemorrhage | Trauma with significant blood loss |
| Gastrointestinal bleeding | |
| Tissue rupture: aortic aneurysm, spleen/ovarian cyst, ectopic pregnancy | |
| Retroperitoneal hemorrhage | |
| Pulmonary embolism | Saddle embolus resulting in outflow tractobstruction or severe hypoxia |
Syncope Rules
In emergency departments, many rules have been established to stratify the risk of a single patient presenting with syncope 14. Examples of such rules are the San Francisco Syncope Rule (SFSR), Osservatorio Epidemiologico sulla Sincope nel Lazio (OESIL), Evaluation of Guidelines in Syncope Study (EGSYS), risk stratification of syncope in the emergency department (Rose), and Boston Syncope Rules. Among these rules, only SFRS had external validity in the systematic review by Saccilotto et al. 15 with the sensitivity of 87% (95%CI 79–93) and specificity of 52% (95% CI 43–62). One of these rules that considers the N-Terminal pro-brain natriuretic peptide (NT-proBNP) and BNP is Rose published in 2010 and derived and validated in a single ED center in Edinburgh 16. The follow-up time of this tool is 30 days, and it is utilized in clinical practices for better and more accurate diagnosis from BNP marker. The criteria for this diagnosis are as follows:
— BNP level ≥300 pg/mL or bradycardia ≤50 in ED or pre-hospital
— Rectal examination showing fecal occult Blood (if suspicion of gastrointestinal Bleeding)
— Anemia: hemoglobin _90 g/L
— Chest pain
— ECG showing Q wave (not in the lead III)
— O2 Saturation ≤94% on room air
Patients are at high risk if a single variable is present.
The sensitivity and specificity for adverse events in this rule are 87% and 56%, respectively 16. Adverse events include pacemaker or cardiac defibrillator implant within 1 month from the index syncope, ventricular tachycardia, acute myocardial infarction, cerebrovascular accidents, life-threatening arrhythmias (ventricular fibrillation, sustained ventricular tachycardia [>120 beats/min], ventricular pause >3 seconds), pulmonary embolism, intracranial or subarachnoid hemorrhage, hemorrhage requiring more than 2 units of blood transfusion, acute surgical procedures, or endoscopic intervention. These rules and biomarkers such as BNP, Troponin, and D-Dimer can diagnose most of the cardiac syncope patients from other types of syncope, and this issue is critical to decreasing the mortality and morbidity of syncope due to cardiac causes.
| Main outcome | Measurement of brain natriuretic peptide concentrations may help confirm cardiac causes of syncope, and merits consideration for incorporation into the algorithm used to Diagnose syncope. | NT-pro-BNP assessment was helpful in differentiating cardiac from non-cardiac syncope. | NT-pro-BNP was a strong and independent diagnostic and prognostic marker and addition to conventional criteria of history and examination improved the discriminatory performance In patients hospitalized for syncope. | BNP may have a role in the risk assessment of syncope patient's in The ED. A BNP cut off of >100 pg/ml has a reasonable sensitivity forserious outcome, while a cut off of >1000 pg/ml has anExcellent positive predictive value and specificity. | Demonstrated that BNP levels are dynamicaround an episode of syncope, rising from baseline to a peakbetween 18 h and 1 week after an episode in many patients. Thereasons for this are not clear. | Measuring BNP and adding ROSE rule to the standardevaluation of syncope can sufficiently predict short-term serious outcomes for patients presenting to EDwith syncope. |
| specificity | 92% | 93.8% | 51.8% | If BNP>100 pg/ml: 69.8% and if BNP>1000 pg/ml:100% | - | - |
| sensitivity | 82% | 90% | 89.7% | If BNP>100 pg/ml: 66.7% and if BNP>1000 pg/ml:33.3% | - | - |
| Cardiac syncope population | 61 | 20 | 78 | - | 5 | - |
| Cut-off value | 40 pg/ml | 164 pg/ml | 156 pg/ml | >100 pg/ml and >1000 pg/ml | - | 250 pg/ml |
| Patient population | 118 | 61 | 161 | 99 | 31 | 41 |
| Study type | Retrospective | Cross-section | Prospective | prospective | prospective | prospective |
| Author/year | Tanimoto (2002) 17 | Pfister (2004) 9 | Pfister (2012) 18 | Reed (2007) 19 | Reed (2010) 16 | Isbitan (2013) 20 |
Diagnostic Value of BNP in Children with Syncope
Syncope is a common problem in children and adolescents. A prevalence rate of 15% has been estimated for the syncopal episode in children under the age of 18 212223. Syncope in children and adolescents can be caused by underlying conditions. The most common type of syncope in children and adolescent is autonomic-mediated reflex syncope (AMS), resulted from the syncope caused by cardiac diseases 242517. About 1-3% of children's and adolescents’ admission in ED is associated with syncope 2517. In our electronic search, we identified two studies on BNP value and syncope in children and adolescents. In a study by Wójtowicz J et al. 24 who evaluated Natriuretic peptides in the children and adolescents with syncope, there was no significant difference in terms of BNP level between the syncope and control groups at all. Their study started with 88 and 25 participants in the syncope and control groups, respectively. The concentration of NT-proBNP in the syncope group was 24.5 pg/mL, and that of NT-proBNP was 4.8pg/mL. In the control group, NT-proBNP and ANP concentrations were 25 pg/mL and 3 pg/mL, respectively, which had no significant difference with the syncope group. Also, the children who were hospitalized due to syncope showed a significant difference in beats per min and a maximum heart rate during the 24-h electrocardiographic Holter monitoring. In another study, Zhang Q et al. 25 evaluated "Diagnostic value of serum brain natriuretic peptide in syncope in children and adolescents." The study concluded that Serum BNP was helpful in differentiating cardiac syncope from non-cardiac syncope in children and adolescents. Sixty-two children and adolescents admitted in ED for syncope were evaluated, among whom 23 participants had cardiac syncope, and 39 had non-cardiac syncope. Regarding BNP levels, there was a significant difference between cardiac syncope (958.78 ± 2443.41 pg/mL) and non-cardiac syncope (31.05 ± 22.64pg/mL) groups (P-value <0.05). Furthermore, a significant difference was observed in terms of mean age, number of predisposing factors during exercise, number of prodromal symptoms and number of Standard ECG abnormalities. The Hypertrophic cardiomyopathy and Cardiac arrhythmia had maximum and minimum values of BNP, respectively (2873.88 ± 4378.15pg/mL and 46.83 ±25.63pg/mL). Other aspects of these studies are presented in Table 2.
Diagnostic Value of BNP in Adults with Syncope
In the electronic search strategy, six studies were identified in which the inclusion criterion was adult syncope. Summaries of these studies are shown in Table 2. A significant difference was found between the mean ages in cardiac syncope compared to non-cardiac syncope in four studies. In the cardiac syncope groups, age was higher than in the non-cardiac syncope ones, and the cause of this relationship was unclear. The results of these studies showed that measuring the BNP level in EDs was very helpful for diagnosis of the individuals with cardiac syncope, and decreased the chance of mortality due to cardiac syncope by using guidelines or rules. Tanimoto K et al. 17 studied BNP for separating cardiac and non-cardiac syncope, and considered the cut-off value of 40 pg/ml for isolating cardiac and non-cardiac syncope with 82% sensitivity and 92% specificity for identification of cardiac syncope. The authors of this study concluded that a significant relationship was found in terms of BNP level between the cardiac group (118±42 pg/ml) and those in the other three groups (Reflex-mediated, Neurologic, and Unknown). Pfister et al. 8 showed that the assessment of NT-pro-BNP was helpful in differentiating cardiac from non-cardiac syncope. A significant difference was observed in BNP level for cardiac group compared to the non-cardiac one (514 pg/ml vs. 182 pg/ml, P-value <0.05). The authors of this study also concluded that the NT-pro-BNP had a high sensitivity and a high negative predictive value for the cardiac cause in patients with syncope and was a better predictor than clinical and ECG features.
Conclusion
We concluded that a biochemical marker such as BNP and other forms of this marker was very helpful in separating and diagnosing cardiac syncope patients and predicting their mortality. This marker, as well as other ones, seem to be very helpful in emergency departments. The accuracy and precision of diagnosing and predicting prognosis of cardiac syncope with Rules were increased. There are few studies on syncope in children, and more studies need to be conducted to clarify the causal relationship.
Recommendations and Future Studies
According to some of the recommendations in previous studies, more research is needed to be conducted to clarify this relationship and the variables that might play the role of confounders in a causal inference. More studies are required on children because there is some controversy in this relationship. And finally, we suggest to study syncope patients with large sample sizes and randomized control trial studies to ensure that this marker is helpful in recognizing and predicting the prognosis of the disease.
Abbreviations
AMS: autonomic-mediated reflex syncope
BNP: Brain Natriuretic Peptides
ECG: electrocardiography
ED: Emergency Department
EGSYS: Evaluation of Guidelines in Syncope Study
ESC: European Society of Cardiology
MI: myocardial infarction
NT-proBNP: N-Terminal pro–brain natriuretic peptide
OESIL: Osservatorio Epidemiologico sulla Sincope nel Lazio
Rose: risk stratification of syncope in the emergency department
SFSR: San Francisco Syncope Rule
Competing Interests
The authors report no conflicts of interest in this work.
Authors' Contributions
Hamideh Feiz Disfani proposed and designed the study, Mostafa Kamani collected the Data and managing manuscripts, Kazem Rahmani contributed in writing and approving the study.
References
-
Reed
M. J.,
Newby
D. E.,
Coull
A. J.,
Prescott
R. J.,
Jacques
K. G.,
Gray
A. J..
The ROSE (risk stratification of syncope in the emergency department) study. Journal of the American College of Cardiology.
2010;
55
:
713-21
.
View Article PubMed Google Scholar -
Pfister
Roman,
Tan
Dajana,
Thekkanal
Jaimy,
Hellmich
Martin,
Schneider
Chistian Alfons.
Predictors of elevated NT-pro-BNP in cardiovascular patients without acute heart failure. International journal of cardiology.
2009;
131
(2)
:
277-280
.
View Article PubMed Google Scholar -
Pfister
R.,
Scholz
M.,
Wielckens
K.,
Erdmann
E.,
Schneider
C. A..
Use of NT-proBNP in routine testing and comparison to BNP. European Journal of Heart Failure.
2004;
6
:
289-93
.
View Article PubMed Google Scholar -
Isbitan
Ahmad,
Hawatmeh
Amer,
Elnahar
Yaser,
Patel
Kunal,
Altheeb
Zaid,
Debari
Vincent,
Hamdan
Ayman,
Shamoon
Fayez.
Utility of brain natriuretic peptide assay as a predictor of short term outcomes in patients presenting with syncope to the emergency department. Cardiovascular diagnosis and therapy.
2016;
6
(3)
:
234
.
View Article PubMed Google Scholar -
Reed
Matthew J,
Newby
David E,
Coull
Andrew J,
Jacques
Keith G,
Prescott
Robin J,
Gray
Alasdair J.
Role of brain natriuretic peptide (BNP) in risk stratification of adult syncope. Emergency Medicine Journal.
2007;
24
(11)
:
769-773
.
PubMed Google Scholar -
Tanimoto
K.,
Yukiiri
K.,
Mizushige
K.,
Takagi
Y.,
Masugata
H.,
Shinomiya
K..
Usefulness of brain natriuretic peptide as a marker for separating cardiac and noncardiac causes of syncope. The American Journal of Cardiology.
2004;
93
:
228-30
.
View Article PubMed Google Scholar -
Brignole
M.,
Alboni
P.,
Benditt
D.,
Bergfeldt
L.,
Blanc
J. J.,
Thomsen
P. E. Bloch,
Syncope
European Society of Cardiology Task Force on.
Guidelines on management (diagnosis and treatment) of syncope. European Heart Journal.
2001;
22
:
1256-306
.
View Article PubMed Google Scholar -
Soteriades
E. S.,
Evans
J. C.,
Larson
M. G.,
Chen
M. H.,
Chen
L.,
Benjamin
E. J..
Incidence and prognosis of syncope. The New England Journal of Medicine.
2002;
347
:
878-85
.
View Article Google Scholar -
Maisel
W. H.,
Stevenson
W. G..
Syncope--getting to the heart of the matter. N Engl J Med.
2002;
347
:
931-933
.
View Article PubMed Google Scholar -
Disfani
H. F.,
Kamandi
M.,
Rahmani
K..
Brain Natriuretic Peptides in Screening of Syncope with Cardiac Origin; a Commentary. Emergency (Tehran, Iran).
2018;
6
.
PubMed Google Scholar -
Kapoor
W. N.,
Karpf
M.,
Wieand
S.,
Peterson
J. R.,
Levey
G. S..
A prospective evaluation and follow-up of patients with syncope. The New England Journal of Medicine.
1983;
309
:
197-204
.
View Article PubMed Google Scholar -
Thiruganasambandamoorthy
V.,
Hess
E. P.,
Turko
E.,
Perry
J. J.,
Wells
G. A.,
Stiell
I. G..
Outcomes in Canadian emergency department syncope patients--are we doing a good job?. The Journal of Emergency Medicine.
2013;
44
:
321-8
.
View Article PubMed Google Scholar -
Fonarow
G. C.,
Peacock
W. F.,
Phillips
C. O.,
Givertz
M. M.,
Lopatin
M.,
Committee
A. S.,
null
null,
Investigators
null.
Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. Journal of the American College of Cardiology.
2007;
49
:
1943-50
.
View Article PubMed Google Scholar -
Pfister
R.,
Tan
D.,
Thekkanal
J.,
Hellmich
M.,
Schneider
C. A..
Predictors of elevated NT-pro-BNP in cardiovascular patients without acute heart failure. International Journal of Cardiology.
2009;
131
:
277-80
.
View Article PubMed Google Scholar -
Tada
H.,
Ito
S.,
Shinbo
G.,
Tadokoro
K.,
Ito
I.,
Hashimoto
T..
Significance and utility of plasma brain natriuretic peptide concentrations in patients with idiopathic ventricular arrhythmias. Pacing and Clinical Electrophysiology.
2006;
29
:
1395-403
.
View Article PubMed Google Scholar -
Sun
B. C.,
Thiruganasambandamoorthy
V.,
Cruz
J. D.,
Standardize
E. D. Syncope Risk Stratification Reporting Consortium to.
Standardized reporting guidelines for emergency department syncope risk-stratification research. Academic Emergency Medicine.
2012;
19
:
694-702
.
View Article PubMed Google Scholar -
Costantino
G.,
Furlan
R..
Syncope risk stratification in the emergency department. Cardiology Clinics.
2013;
31
:
27-38
.
View Article Google Scholar -
Moya
A.,
Sutton
R.,
Ammirati
F.,
Blanc
J. J.,
Brignole
M.,
Dahm
J. B.,
Task Force for the
Diagnosis,
Management of
Syncope,
European Society of
Cardiology,
European Heart Rhythm
Association,
Heart Failure
Association,
Heart Rhythm
Society.
Guidelines for the diagnosis and management of syncope (version 2009). European Heart Journal.
2009;
30
:
2631-71
.
View Article Google Scholar -
Grossman
S. A.,
Babineau
M.,
Burke
L.,
Kancharla
A.,
Mottley
L.,
Nencioni
A..
Do outcomes of near syncope parallel syncope?. The American Journal of Emergency Medicine.
2012;
30
:
203-6
.
View Article PubMed Google Scholar -
Saccilotto
Ramon T.,
Nickel
Christian H.,
Bucher
Heiner C.,
Steyerberg
Ewout W.,
Bingisser
Roland,
Koller
Michael T..
San Francisco Syncope Rule to predict short-term serious outcomes: a systematic review. Canadian Medical Association Journal.
2011;
183
:
E1116-E1126
.
View Article PubMed Google Scholar -
Driscoll
D. J.,
Jacobsen
S. J.,
Porter
C. J.,
Wollan
P. C..
Syncope in children and adolescents. Journal of the American College of Cardiology.
1997;
29
:
1039-45
.
View Article Google Scholar -
Massin
M. M.,
Bourguignont
A.,
Coremans
C.,
Comte
L.,
Lepage
P.,
Gerard
P..
Syncope in pediatric patients presenting to an emergency department. The Journal of Pediatrics.
2004;
145
:
223-8
.
View Article Google Scholar -
Wieling
W.,
Ganzeboom
K. S.,
Saul
J. P..
Reflex syncope in children and adolescents. Heart (British Cardiac Society).
2004;
90
:
1094-100
.
View Article Google Scholar -
Wojtowicz
J.,
Szczepanski
W.,
Bogdan
A.,
Baran
M.,
Szczurak
J.,
Bossowski
A..
Natriuretic peptides in the evaluation of syncope in children and adolescents. Scandinavian Journal of Clinical and Laboratory Investigation.
2014;
74
:
301-5
.
View Article Google Scholar -
Zhang
Q.,
Jin
H.,
Qi
J.,
Yan
H.,
Du
J..
Diagnostic value of serum brain natriuretic peptide in syncope in children and adolescents. Acta Paediatrica (Oslo, Norway).
2013;
102
:
e210-4
.
View Article PubMed Google Scholar
Comments
Downloads
Article Details
Volume & Issue : Vol 5 No 12 (2018)
Page No.: 2904-2909
Published on: 2018-12-25
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 5227 times
- Download PDF downloaded - 1215 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress

