Abstract
Background: Results from the latest meta-analysis, in fresh cycles, showed that the application of time-lapse monitoring (TLM) together with an embryo-evaluating algorithm was associated with a significantly higher rate of ongoing pregnancy and a lower rate of early pregnancy loss. The aim of this study was to compare the clinical outcomes of frozen embryos classified according to morphokinetic versus morphologic criteria.
Methods: This was a retrospective cohort study, conducted at IVFAS, An Sinh Hospital, Vietnam, from July 2014 to July 2017. Patients undergoing in vitro fertilization (IVF) treatment with antagonist protocol and having freeze-only on day 5 were included. Exclusion criteria were patients (i) treated with in-vitro maturation, (ii) having obstructive azoospermia, or (iii) having uterine abnormalities. Embryos were cultured up to day 5 in TLM system (Primo Vision, Vitrolife, Sweden) or in benchtop (G185, K System, Denmark). The quality of frozen embryos was evaluated based on morphokinetic or morphologic criteria. In the subsequent cycle, endometrial preparation was done by using exogenous estradiol and progesterone. Embryos were thawed and up to 2 embryos were transferred to the uterus. The primary outcome was ongoing pregnancy. The rate of post-thaw survival, post-thawed good/moderate embryo, clinical pregnancy, implantation, miscarriage and ectopic pregnancy were used as secondary endpoints.
Results: A total of 276 patients were recruited, with 138 patients in the morphokinetic group and 138 patients in the morphologic group. Baseline characteristics were comparable between the two groups. There was no significant difference in ongoing pregnancy rate in morphokinetic versus morphologic group (57.2% vs. 60.1%, p=0.71). All secondary outcomes were comparable between the two groups.
Conclusion: In frozen day-5 embryo transfer, the clinical outcomes were similar when embryos were classified according to morphokinetic versus morphologic criteria for freezing. Using morphokinetic criteria to select embryos for freezing did not improve the ongoing pregnancy rate, as compared to morphologic criteria.
Introduction
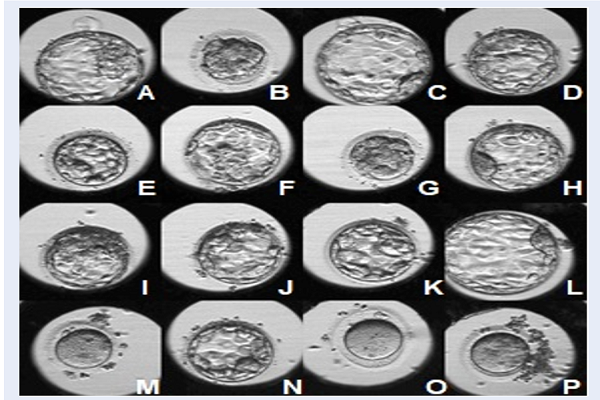
Embryo culture, assessment and selection are important steps in improvement of the safety and efficacy in assisted reproductive technology. Traditionally, an embryo must be removed from an incubator for assessing under a light microscope; its development may be affected from exposure to ambient temperature and pH conditions 1. Embryos were evaluated and classified at the time of embryo assessment, based on morphologic criteria including cell numbers, fragmentation rate, nucleation status, cytoplasmic anomalies, spatial distribution of cells, compaction status in cleavage embryo and degree of expansion, inner cell mass morphology, and trophectoderm morphology in blastocysts. In recent years, embryo culture combined with time-lapse monitoring has become more popular worldwide and has created a new trend of in vitro fertilization 234. It can maintain an optimal culture environment, and allow for the best possible culture conditions 56. Time-lapse system can take digital images of embryos at frequent time intervals throughout the culture period so that the embryos can be quality-assessed without being removed from the incubator Figure 1.
Time-lapse systems also record the data of embryo development (morphokinetics), including the precise determination of the onset, duration, and interval between cell divisions. In addition, dynamic morphologic characteristics of a developing human embryo, such as pronuclei (PN) and nucleus formation and disappearance, fragmentation, and size distribution of blastomeres may be quantified with time-lapse monitoring 78. Based on the recorded data, potential embryos are used to classify and select with the support of time-lapse software.
These recent findings suggested that morphokinetic parameters may supplement current embryo selection methods to possibly increase clinical pregnancy rates for in vitro fertilization (IVF) treatments 791011. Meanwhile, other studies reported no significant differences in embryo incubation and selection between the time-lapse incubator and conventional incubator 1213. Pribenszky et al. recently updated their meta-analysis review and found that the quality of the evidence was moderate to low and that there were inconsistencies across the studies. Selective application and variability were also limitations. Although time-lapse is shown to significantly improve overall clinical outcome, further high-quality evidence are needed before conclusions can be drawn 14.
Recently, there has been greater evidence supporting elective frozen embryo transfer and its improved clinical outcomes, which not only achieved higher pregnancy rates but also lowered maternal and infant morbidity and mortality 15. Frozen embryo transfer has become increasingly popular worldwide. Nevertheless, most of the published studies have mainly analyzed morphokinetic data in embryo selection in fresh embryo transfer cycles 13161718. Therefore, it was necessary to verify the effectiveness of the morphokinetic criteria in embryo selection for freezing at our center. Accordingly, the aim of our study was to compare the clinical outcomes of frozen embryos classified according to morphokinetic versus morphologic criteria.
Methods
Patient population and study design
This is a retrospective cohort study which was conducted at IVFAS (An Sinh Hospital, Vietnam) from July 2014 to July 2017. The identifying information was removed from patient data. As the data cannot be linked back to an individual, it was not necessary to obtain patient consent. The use of patient data was approved by An Sinh Hospital. All patients undergoing IVF treatment with antagonist protocol and having freeze-only embryo on day 5 were included in our study. Patients undergoing in vitro maturation (IVM) cycles, having obstructive azoospermia or having any uterine abnormalities were excluded. In this study, 256 patients undergoing assisted reproduction technology were recruited. The patients were grouped into morphokinetic group (138 patients) and morphologic group (138 patients).
Embryo culture
After retrieval, oocytes were rinsed and cultured in G-IVF Plus (Vitrolife, Sweden) at 37°C with 6% CO2, 5% O2 in incubator (Galaxy 170R, New Brunswick) 19. After 2 hours, denudation of cumulus cells surrounding the oocytes was performed by Pasteur pipette and Hyase (Vitrolife, Sweden) 19. Subsequently, intracytoplasmic sperm injection (ICSI) was performed with all mature oocytes. After ICSI, oocytes were cultured overnight in G1 – Plus media (Vitrolife, Sweden) at 37°C with 6% CO2, 5% O2 in benchtop (G185, K System, Denmark) 20. Fertilization was checked approximately 16 to 18 hours after ICSI 21.
Conventional embryo culture
Three days after ICSI, all embryos were transferred to G2 – Plus media (Vitrolife, Sweden) for culturing at 37°C with 6% CO2, 5% O2 in benchtop (G185, K System, Denmark) to blastocysts (20).
Time-lapse embryo culture
After evaluation of the fertilization, embryos were transferred to WOW dish with G-TL media (Vitrolife, Sweden) and placed in Primo Vision time-lapse system (Vitrolife, Sweden) which was placed in an incubator at 37°C with 6% CO2, 5% O2 (Galaxy 170R, New Brunswick).
Embryo evaluation
Conventional embryo culture
On day 5 after oocyte retrieval, embryos were removed from the incubator for quality assessment, under a light microscope, based on three main features: the degree of expansion, inner cell mass (ICM) morphology and trophectoderm (TE) morphology 22. The timing of embryo assessment on day 5 was 116 ± 2 hours after ICSI.
Time-lapse embryo culture
Every embryo was assessed based on morphologic criteria and morphokinetic parameters. The whole development process of embryos was observed via the monitor of Primo Vision time-lapse system. The timing of embryo cleavage and appearance of abnormal characteristics were marked. Specific kinetic markers were evaluated: time to pronuclear (2PN) fading (t1) and cleavage to 2 cells, 3 cells, 4 cells, 5 cells, 8 cells, morula (t2, t3, t4, t5, t8, tM), time of embryo to start of blastulation, expanded blastocyst, and time of hatching (tEB, tB, tH.Blast). The abnormalities in the cleavage stage embryo were also marked at the time of occurrence and included: reverse cleavage (RCLV — decrease of the number of embryos during division), direct cleavage (DC — a single blastomere directly cleaved into three or more blastomeres), and MNB (multinucleated blastomeres) 23.
Moreover, kinetic parameters were calculated based on the time of the listed events, including: duration of the second cycle (cc2; t3 — t2), third cell cycle (cc3; t5 - t3), time of synchronous divisions s2 (t4 — t3), and s3 (t8 — t5) 13242526.
Embryo selection
Morphologic group
Embryo selection for freezing was based on embryo morphologic criteria (Istanbul consensus workshop on embryo assessment in 2011) 22. Selected embryos for freezing had expansion grade from 2 to 5, ICM category 1 or 2, TE category 1 or 2 22.
Morphokinetic group
Embryos were selected for freezing based on morphologic criteria, timing of kinetic events, and presence of cleavage anomalies 26. Morphokinetic parameters were referenced from the study of Meseguer et al. (2011) and installed in Primo Vision software 26. When selecting embryos, embryos were sorted in order by the software based on the parameters that had been installed.
Embryo freezing
In two group, embryos had been frozen using the Cryotec vitrification method, with a maximum of two embryos per cryotec.
Vitrification protocol
Preparation
Preparation of the solution in vitriplate included: 300 µL equilibration solution (ES), 600 µL vitrification solution (VS) and then divide VS to the next two wells, VS1 (300 μL) and VS2 (300 μL). Then, they were placed at room temperature (25°C - 27°C) for at least 1 hour before use.
Freezing
Freezing protocol included 3 steps: equilibration (maximum 15 minutes), vitrification 1 (30 – 40 seconds), vitrification 2 (10 – 20 seconds) (following the manufacturer's protocol). The details are as below:
Put embryo on the surface of ES in ES well for a maximum of 15 minutes. Then, transfer embryo to the half depth of the VS1 well for 30 – 40 seconds. Transfer embryo to the half depth of the VS2 well for 10 – 20 seconds. Finally, put it on the end of the Cryotec seat with a minimum volume of VS and immediately submerge the Cryotec into liquid nitrogen.
Warming protocol
Preparation
The TS dish and the TS vial (with closed cap) were placed in the incubator at 37°C overnight before use. Preparation of the solution in vitriplate included: 300 μL of diluent solution (DS) in the first well, 600 μL washing solution (WS) and then divide WS to the next two wells, WS1 (300 μL) and WS2 (300 μL). They were placed at room temperature (25°C — 27°C) for at least 1 hour before use.
Warming
The warming protocol included 3 steps: warming (1 minute), dilution (3 minutes), washing 1 (5 minutes) and washing 2 (1 minute) (following the manufacturer's protocol). The details are as below:
Take the TS vial out of the incubator, and expel all of it to the TS dish. Quickly put the Cryotec from liquid nitrogen into the TS dish. Let the embryo release from the Cryotec and wait for 1 minute. Transfer the embryo to the bottom of the DS well and wait for 3 minutes. Transfer the embryo to the bottom of the WS1 and then wait for 5 minutes. Transfer the embryo on the surface of the WS2, and wait for 1 minute. Put the embryo into the droplet of culture media until the embryo transfer step.
Embryo transfer and outcome measures
Endometrial preparation was done by using exogenous estradiol and progesterone until the endometrial thickness reached 8 mm or more. After 5 days from the start of progesterone, embryos were thawed (up to 2 embryos). Two hours after thawing, the embryo was transferred to the uterus under ultrasonographic guidance.
The primary outcome was ongoing pregnancy after the first embryo transfer cycle. The ongoing pregnancy was defined as pregnancy with a detectable heart rate after 12 weeks of gestation 2728. The secondary outcomes were the percentage of survival, clinical pregnancy, implantation, miscarriage and ectopic pregnancy.
Statistical analysis
The samples of the two groups were matched by MatchED Packages (R software). The results were compared depending on embryo evaluation criteria by using a Chi-squared test and significance level of p < 0.05. All the statistical analyses were performed using R software.
Results
All of the baseline characteristics of the patients were recorded including age, BMI, infertility duration, total FSH dose, and total days of stimulation. These characteristics were summarized in Table 1.
| Characteristic | Morphokinetic group n = 138 | Morphologic group n = 138 | p-value |
| Age (years) | 31.9 ± 5.1 | 32.3 ± 5.9 | 0.65 |
| BMI (kg/m 2 ) | 21.1 ± 2.2 | 21.1 ± 2.1 | 0.76 |
| Infertility duration (years) | 5.0 ± 3.2 | 5.3 ± 4.1 | 0.66 |
| Total FSH dose (IU) | 2206.8 ± 1065.7 | 2341.5 ± 971.2 | 0.29 |
| Total days of stimulation (days) | 9.0 ± 2.1 | 8.7 ± 1.5 | 0.20 |
The morphokinetic group showed similar age (31.9 ± 5.1 years vs. 32.3 ± 5.9 years, p = 0.65), infertility duration (5.0 ± 3.2 years vs. 5.3 ± 4.1 years, p = 0.66) and total FSH dose (2206.8 ± 1065.7 IU vs. 2341.5 ± 971.2 IU, p = 0.29), as compared to the morphologic group. There were no significant differences between the two groups (Table 1). This was evident by the fact that the primary patient’s characteristics were similar between the two groups.
From all of the patients, there were a total of 6,264 retrieved oocytes with 5,369 mature oocytes which were administered with intracytoplasmic sperm injection. The fertilization rate reached 84.4%. The morphokinetic group showed a similar average number of retrieved oocytes (22.9 ± 9.8 vs. 22.5 ± 9.4 oocytes, p = 0.74, ICSI oocytes (19.6 ± 8.7 vs. 19.3 ± 8.0 oocytes, p = 0.77), fertilized oocytes (14.4 ± 7.0 vs. 14.7 ± 6.8 oocytes, p = 0.70), day-5 embryos (13.7 ± 6.8 vs. 13.0 ± 6.6 embryos, p = 0.40), and frozen embryos (5.6 ± 3.6 vs. 5.6 ± 3.2 embryos, p=0.99), as compared to the morphologic group (Table 2).
| Parameters | Morphokinetic group n = 138 | Morphologic group n = 138 | p-value |
| Number of retrieved oocytes | 22.9 ± 9.8 | 22.5 ± 9.4 | 0.74 |
| Numbers of ICSI oocytes | 19.6 ± 8.7 | 19.3 ± 8.0 | 0.77 |
| Number of fertilized oocytes | 14.4 ± 7.0 | 14.7 ± 6.8 | 0.70 |
| Number of day-5 embryos | 13.7 ± 6.8 | 13.0 ± 6.6 | 0.40 |
| Number of frozen embryos | 5.6 ± 3.6 | 5.6 ± 3.2 | 0.99 |
Our primary outcome (ongoing pregnancy rate) was found in 57.2% in the morphokinetic group, compared to 60.1% in the morphologic group, and it was not significantly different between the two groups. The morphokinetic group showed similar number of embryos transferred (1.9 ± 0.4 vs. 2.0 ± 0.3 embryos, p = 0.74) and clinical pregnancy rate (64.5% vs. 65.9%, p = 0.90), as compared to the morphologic group. There were no statistically significant differences in mean of endometrial thickness (11.0 ± 1.2 mm vs. 10.8 ± 1.3 mm, p = 0.09), implantation rate (51.2% vs. 49.3%, p = 0.73), or ectopic pregnancy rate (2.9% vs. 0.7%, p = 0.37) between the two groups. Besides, the two groups were equal in the post-thawing survival embryo rate (100%) and miscarriage rate (5.1%) (Table 3).
| Parameter | Morphokinetic group n = 138 | Morphologic group n = 138 | p-value |
| Post-thawing survival rate (%) | 100 | 100 | 1.00 |
| Endometrial thickness on FET day (mm) | 11.0 ± 1.2 | 10.8 ± 1.3 | 0.09 |
| Number of embryos transferred | 1.9 ± 0.4 | 2.0 ± 0.3 | 0.74 |
| Ongoing pregnancy rate (%) | 57.2 | 60.1 | 0.71 |
| Clinical pregnancy rate (%) | 64.5 | 65.9 | 0.90 |
| Implantation rate (%) | 51.2 | 49.3 | 0.73 |
| Miscarriage rate (%) | 5.1 | 5.1 | 1.00 |
| Ectopic pregnancy rate (%) | 2.9 | 0.7 | 0.37 |
Discussion
Embryos were evaluated based on their morphologic characteristics 22, a practiced routinely applied in many IVF centers worldwide. In this criteria, blastocyst transfer with fewer embryos can be performed with high implantation and clinical pregnancy rates 293031. Morphokinetic data, recorded through time-lapse technology, help make the embryologist’s selection more precise and improve clinical outcomes 3233. Extended culture to blastocyst stage has been a new trend that has been applied in many IVF centers around the world, including Vietnam 3435. Vitrification technologies have been widely used in embryo freezing and the clinical outcomes have been very good 3637. Frozen embryo transfer has increased worldwide and predominated in all embryo transfer cycles 15.
This was the first study to evaluate the effectiveness of morphokinetic criteria in day-5 embryo selection in the first frozen embryo transfer cycle after freeze-all embryo in Vietnamese patients. There were no statistically significant differences in the mean of age, BMI, infertility duration, total FSH dose and total days of stimulation (Table 1). The number of retrieved oocytes, the numbers of mature oocytes using to performance of ICSI, the number of fertilized oocytes, the number of day-5 embryos and day-5 frozen embryos were recorded and analyzed. There were no statistically significant differences between the morphokinetic group versus morphologic group. The above analysis showed that there were similarities between the two groups in terms of patient characteristics and laboratory outcomes.
In this study, we froze all potential embryos conceived during the IVF cycle. By using Cryotec method (Reprolife, Japan), vitrification and thawing embryo protocol were applied correctly, so the post-thawing survival embryo rate was up to 100% in both groups. To ensure endometrial acceptability, endometrial thickness was assessed by the doctor before embryo transfer; this parameter was similar in the two groups.
The results of our study showed that there was no statistically significant difference between the morphokinetic group versus morphologic group. The ongoing pregnancy rate was relatively high (57.2% vs. 60.1%, p = 0.71). Recently, the predictive value of morphokinetic parameters has been studied 13263839404142. Our study was a retrospective cohort study which was compiled data from July 2014 to July 2017. All potential embryos were frozen and our clinical outcomes were analyzed based on the patient's first frozen embryo transfer cycle. Previous studies have been published; although their clinical outcomes were analyzed on the fresh embryo transfer cycle, they were similar to our study. In 2014, Rubio et al. used time-lapse system in embryo culture, selected embryos based on multivariable morphokinetic model, and reproductive outcomes were compared to embryo selection based on morphology. In this study, Rubio et al. conducted a prospective, randomized, double-blinded, controlled study which included eight hundred forty-three infertile couples undergoing ICSI. They concluded that reproductive outcomes were improved when using time-lapse system in culture and selection embryo based on embryo morphokinetic criteria. However, the ongoing pregnancy was not statistically significant different between the two groups (morphokinetic vs. morphologic criteria in embryo selection) 10. Recently, in another prospective cohort study, there was a total of 235 patients who underwent fresh autologous IVF cycles. They were divided into 2 groups: time-lapse monitoring (119 patients) and conventional morphologic embryo screening (116 patients). There was no statistically significant difference between two groups in clinical pregnancy and implantation rates 13.
Some studies only analyzed cleavage embryo selection in order to compare the effectiveness of morphokinetic versus morphologic criteria in embryo selection 91643. Wu et al. analyzed a total of 608 patients, which was divided into two equal groups (time-lapse and standard incubator culture system) with 304 patients in each group. They found that the ongoing pregnancy rate and the live birth rate in time-lapse group were higher than that of the standard incubator culture system 16. Siristatidis showed in a study population (of 239 women) that the women were classified into two groups: time-lapse and conventional monitoring. The clinical and ICSI cycle characteristics and reproductive outcomes were compared. The results showed better reproductive outcomes in the time-lapse monitoring group 9.
From the results of the above studies, when embryo selection was done using the morphokinetic criteria, the clinical outcomes were not the same between the cleavage embryos and blastocysts. A possible cause is the chromosome self-normalization during the development from embryo to blastocyst stage 44.
Recently, Chen et al. published a review of effectiveness of time-lapse imaging versus conventional methods in culture and embryo selection in clinical in-vitro fertilization 45. Currently there is insufficient evidence to support that time-lapse is better than conventional methods. To evaluate the effectiveness of time-lapse imaging, more well-designed randomized clinical trials need to be done 45.
The limitation of our study is that it was a retrospective cohort study, in which we did not actively select samples for the study. Instead, we collected data on treated outcomes of the patient.
Conclusions
The clinical outcomes of frozen embryo transfer were similar when embryos were classified according to morphokinetic versus morphologic criteria for freezing. Using morphokinetic criteria to select day-5 embryo for freezing did not improve the ongoing pregnancy rate, as compared to morphologic criteria. Our study design was weak and sample size may not be large enough to make a statistically significant difference. A more well-designed study with a larger sample size needs to be considered and may provide impactful results.
Abbreviations
BMI: Body Mass Index
FET: Frozen embryo transfer
FSH: Follicle stimulating hormone
ICSI: Intracytoplasmic sperm injection
IVF: In-vitro fertilization
IVM: In-vitro maturation
RCT: Randomized controlled trial
TLM: Time-lapse monitoring
Competing Interests
The authors declare that they have no conflict of interests.
Authors' Contributions
LNQ drafted the manuscript. LNQ, LTBT and NHMT performed the IVF, embryo vitrification works. DQV planned and designed the experiments. PDT, LNQ collected and analysed the data. NTTH supervised the study and finalized the manuscript. All authors read and approved the final manuscript.
Acknowledgments
This study use data of IVFAS, An Sinh Hospital. We are thankful to our colleagues from IVFAS who greatly assisted to complete the study.
References
-
Fujiwara
M.,
Takahashi
K.,
Izuno
M.,
Duan
Y. R.,
Kazono
M.,
Kimura
F..
Effect of micro-environment maintenance on embryo culture after in-vitro fertilization: comparison of top-load mini incubator and conventional front-load incubator. Journal of Assisted Reproduction and Genetics.
2007;
24
:
5-9
.
View Article PubMed Google Scholar -
Pribenszky
C.,
Matyas
S.,
Kovacs
P.,
Losonczi
E.,
Zadori
J.,
Vajta
G..
Pregnancy achieved by transfer of a single blastocyst selected by time-lapse monitoring. Reproductive Biomedicine Online.
2010;
21
:
533-6
.
View Article PubMed Google Scholar -
Cruz
M.,
Gadea
B.,
Garrido
N.,
Pedersen
K. S.,
Martinez
M.,
Perez-Cano
I..
Embryo quality, blastocyst and ongoing pregnancy rates in oocyte donation patients whose embryos were monitored by time-lapse imaging. Journal of Assisted Reproduction and Genetics.
2011;
28
:
569-73
.
View Article PubMed Google Scholar -
Kovacic
B.,
Hojnik
N.,
Vlaisavljevic
V..
The use of time lapse photography in an in vitro fertilization programme for better selection for embryo transfer. Journal of Stem Cells.
2014;
9
:
39-52
.
PubMed Google Scholar -
Zhang
J. Q.,
Li
X. L.,
Peng
Y.,
Guo
X.,
Heng
B. C.,
Tong
G. Q..
Reduction in exposure of human embryos outside the incubator enhances embryo quality and blastulation rate. Reproductive Biomedicine Online.
2010;
20
:
510-5
.
View Article PubMed Google Scholar -
Wong
C.,
Chen
A. A.,
Behr
B.,
Shen
S..
Time-lapse microscopy and image analysis in basic and clinical embryo development research. Reproductive Biomedicine Online.
2013;
26
:
120-9
.
View Article PubMed Google Scholar -
Meseguer
Marcos,
Rubio
Irene,
Cruz
Maria,
Basile
Natalia,
Marcos
Julian,
Requena
Antonio.
Embryo incubation and selection in a time-lapse monitoring system improves pregnancy outcome compared with a standard incubator: a retrospective cohort study. Fertility and Sterility.
2012;
98
:
1481-1489.e10
.
View Article PubMed Google Scholar -
Kirkegaard
K.,
Agerholm
I. E.,
Ingerslev
H. J..
Time-lapse monitoring as a tool for clinical embryo assessment. Human Reproduction (Oxford, England).
2012;
27
:
1277-85
.
View Article PubMed Google Scholar -
Siristatidis
C.,
Komitopoulou
M. A.,
Makris
A.,
Sialakouma
A.,
Botzaki
M.,
Mastorakos
G..
Morphokinetic parameters of early embryo development via time lapse monitoring and their effect on embryo selection and ICSI outcomes: a prospective cohort study. Journal of Assisted Reproduction and Genetics.
2015;
32
:
563-70
.
View Article PubMed Google Scholar -
Rubio
Irene,
Galán
Arancha,
Larreategui
Zaloa,
Ayerdi
Fernando,
Bellver
Jose,
Herrero
Javier,
Meseguer
Marcos.
Clinical validation of embryo culture and selection by morphokinetic analysis: a randomized, controlled trial of the EmbryoScope. Fertility and Sterility.
2014;
102
:
1287-1294.e5
.
View Article PubMed Google Scholar -
VerMilyea
M. D.,
Tan
L.,
Anthony
J. T.,
Conaghan
J.,
Ivani
K.,
Gvakharia
M..
Computer-automated time-lapse analysis results correlate with embryo implantation and clinical pregnancy: a blinded, multi-centre study. Reproductive Biomedicine Online.
2014;
29
:
729-36
.
View Article PubMed Google Scholar -
Kirkegaard
K.,
Hindkjaer
J. J.,
Grondahl
M. L.,
Kesmodel
U. S.,
Ingerslev
H. J..
A randomized clinical trial comparing embryo culture in a conventional incubator with a time-lapse incubator. Journal of Assisted Reproduction and Genetics.
2012;
29
:
565-72
.
View Article PubMed Google Scholar -
Goodman
Linnea R,
Goldberg
Jeffrey,
Falcone
Tommaso,
Austin
Cynthia,
Desai
Nina.
Does the addition of time-lapse morphokinetics in the selection of embryos for transfer improve pregnancy rates? A randomized controlled trial. Fertility and Sterility.
2016;
105
:
275-285. e10
.
View Article PubMed Google Scholar -
Pribenszky
C.,
Nilselid
A. M.,
Montag
M..
Time-lapse culture with morphokinetic embryo selection improves pregnancy and live birth chances and reduces early pregnancy loss: a meta-analysis. Reproductive Biomedicine Online.
2017;
35
:
511-20
.
View Article PubMed Google Scholar -
Evans
J.,
Hannan
N. J.,
Edgell
T. A.,
Vollenhoven
B. J.,
Lutjen
P. J.,
Osianlis
T..
Fresh versus frozen embryo transfer: backing clinical decisions with scientific and clinical evidence. Human Reproduction Update.
2014;
20
:
808-21
.
View Article PubMed Google Scholar -
Wu
L.,
Han
W.,
Wang
J.,
Zhang
X.,
Liu
W.,
Xiong
S..
Embryo culture using a time-lapse monitoring system improves live birth rates compared with a conventional culture system: a prospective cohort study. Human Fertility.
2017;
ooo
:
1-8
.
-
Yu
C. H.,
Zhang
R. P.,
Li
J.,
A
Z. C..
A predictive model for high-quality blastocyst based on blastomere number, fragmentation, and symmetry. Journal of Assisted Reproduction and Genetics.
2018;
35
:
809-16
.
View Article PubMed Google Scholar -
Park
H.,
Bergh
C.,
Selleskog
U.,
Thurin-Kjellberg
A.,
Lundin
K..
No benefit of culturing embryos in a closed system compared with a conventional incubator in terms of number of good quality embryos: results from an RCT. Human Reproduction (Oxford, England).
2015;
30
:
268-75
.
View Article Google Scholar -
Granot
I.,
Dekel
N..
Textbook of Assisted Reproductive TechniquesTaylor & Francis 2012.
Google Scholar -
Gardner
D. K.,
Lane
M..
2012.
View Article Google Scholar -
Ebner
T..
2012.
View Article Google Scholar -
Balaban
B.,
Brison
D.,
Calderon
G.,
Catt
J.,
Conaghan
J.,
Cowan
L.,
Alpha Scientists in Reproductive
Medicine,
The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Human Reproduction (Oxford, England).
2011;
26
:
1270-83
.
View Article Google Scholar -
Rubio
I.,
Kuhlmann
R.,
Agerholm
I.,
Kirk
J.,
Herrero
J.,
Escriba
M. J..
Limited implantation success of direct-cleaved human zygotes: a time-lapse study. Fertility and Sterility.
2012;
98
:
1458-63
.
View Article Google Scholar -
Chamayou
S.,
Patrizio
P.,
Storaci
G.,
Tomaselli
V.,
Alecci
C.,
Ragolia
C..
The use of morphokinetic parameters to select all embryos with full capacity to implant. Journal of Assisted Reproduction and Genetics.
2013;
30
:
703-10
.
View Article Google Scholar -
Campbell
A..
Atlas Of Time Lapse Embryology 2015.
View Article Google Scholar -
Meseguer
M.,
Herrero
J.,
Tejera
A.,
Hilligsoe
K. M.,
Ramsing
N. B.,
Remohi
J..
The use of morphokinetics as a predictor of embryo implantation. Human Reproduction (Oxford, England).
2011;
26
:
2658-71
.
View Article Google Scholar -
Yi
Y.,
Lu
G.,
Ouyang
Y.,
lin
G.,
Gong
F.,
Li
X..
A logistic model to predict early pregnancy loss following in vitro fertilization based on 2601 infertility patients. Reproductive Biology and Endocrinology.
2016;
14
:
15
.
View Article Google Scholar -
Singh
N.,
Goyal
M.,
Malhotra
N.,
Tiwari
A.,
Badiger
S..
Predictive value of early serum beta-human chorionic gonadotrophin for the successful outcome in women undergoing in vitro fertilization. Journal of Human Reproductive Sciences.
2013;
6
:
245-7
.
View Article Google Scholar -
Mangalraj
A. M.,
Muthukumar
K.,
Aleyamma
T.,
Kamath
M. S.,
George
K..
Blastocyst stage transfer vs cleavage stage embryo transfer. Journal of Human Reproductive Sciences.
2009;
2
:
23-6
.
View Article Google Scholar -
Sotiroska
V.,
Petanovski
Z.,
Dimitrov
G.,
Hadji-Lega
M.,
Shushleski
D.,
Saltirovski
S..
The day of embryo transfer affects delivery rate, birth weights, female-to-male ratio, and monozygotic twin rate. Taiwanese Journal of Obstetrics & Gynecology.
2015;
54
:
716-21
.
View Article Google Scholar -
Gardner
D. K.,
Lane
M.,
Stevens
J.,
Schlenker
T.,
Schoolcraft
W. B..
Blastocyst score affects implantation and pregnancy outcome: towards a single blastocyst transfer. Fertility and Sterility.
2000;
73
:
1155-8
.
View Article Google Scholar -
Kovacs
P..
Embryo selection: the role of time-lapse monitoring. Reproductive Biology and Endocrinology.
2014;
12
:
124
.
View Article Google Scholar -
Basile
N.,
Caiazzo
M.,
Meseguer
M..
What does morphokinetics add to embryo selection and in-vitro fertilization outcomes?. Current Opinion in Obstetrics & Gynecology.
2015;
27
:
193-200
.
View Article PubMed Google Scholar -
Sepulveda
S. J.,
Portella
J. R.,
Noriega
L. P.,
Escudero
E. L.,
Noriega
L. H..
Extended culture up to the blastocyst stage: a strategy to avoid multiple pregnancies in assisted reproductive technologies. Biological Research.
2011;
44
:
195-9
.
View Article Google Scholar -
Quea
G.,
Romero
K.,
Garcia-Velasco
J. A..
Extended embryo culture to increase implantation rate. Reproductive Biomedicine Online.
2007;
14
:
375-83
.
View Article Google Scholar -
Basile
N.,
Garcia-Velasco
J. A..
The state of “freeze-for-all“ in human ARTs. Journal of Assisted Reproduction and Genetics.
2016;
33
:
1543-50
.
View Article PubMed Google Scholar -
Roque
M..
Freeze-all policy: is it time for that?. Journal of Assisted Reproduction and Genetics.
2015;
32
:
171-6
.
View Article Google Scholar -
Canto
M. Dal,
Coticchio
G.,
Renzini
M. Mignini,
Ponti
E. De,
Novara
P. V.,
Brambillasca
F..
Cleavage kinetics analysis of human embryos predicts development to blastocyst and implantation. Reproductive Biomedicine Online.
2012;
25
:
474-80
.
View Article PubMed Google Scholar -
Adolfsson
E.,
Porath
S.,
Andershed
A. N..
External validation of a time-lapse model; a retrospective study comparing embryo evaluation using a morphokinetic model to standard morphology with live birth as endpoint. JBRA Assisted Reproduction.
2018;
22
:
205-14
.
View Article Google Scholar -
Adolfsson
E.,
Andershed
A. N..
Morphology vs morphokinetics: a retrospective comparison of inter-observer and intra-observer agreement between embryologists on blastocysts with known implantation outcome. JBRA Assisted Reproduction.
2018;
22
:
228-37
.
View Article Google Scholar -
Azzarello
A.,
Hoest
T.,
Mikkelsen
A. L..
The impact of pronuclei morphology and dynamicity on live birth outcome after time-lapse culture. Human Reproduction (Oxford, England).
2012;
27
:
2649-57
.
View Article PubMed Google Scholar -
Hlinka
D.,
Kalatova
B.,
Uhrinova
I.,
Dolinska
S.,
Rutarova
J.,
Rezacova
J..
Time-lapse cleavage rating predicts human embryo viability. Physiological Research.
2012;
61
:
513-25
.
PubMed Google Scholar -
Adamson
G. David,
Abusief
Mary E.,
Palao
Lourella,
Witmer
Jennifer,
Palao
Lonyl M.,
Gvakharia
Marina.
Improved implantation rates of day 3 embryo transfers with the use of an automated time-lapse–enabled test to aid in embryo selection. Fertility and Sterility.
2016;
105
:
369-375.e6
.
View Article Google Scholar -
Munne
S.,
Velilla
E.,
Colls
P.,
Bermudez
M. Garcia,
Vemuri
M. C.,
Steuerwald
N..
Self-correction of chromosomally abnormal embryos in culture and implications for stem cell production. Fertility and Sterility.
2005;
84
:
1328-34
.
View Article PubMed Google Scholar -
Chen
M.,
Wei
S.,
Hu
J.,
Yuan
J.,
Liu
F..
Does time-lapse imaging have favorable results for embryo incubation and selection compared with conventional methods in clinical in vitro fertilization? A meta-analysis and systematic review of randomized controlled trials. PLoS One.
2017;
12
:
e0178720
.
View Article PubMed Google Scholar
Comments
Downloads
Article Details
Volume & Issue : Vol 5 No 12 (2018)
Page No.: 2910-2917
Published on: 2018-12-26
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 8553 times
- Download PDF downloaded - 1554 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress


