Abstract
Introduction: One of the concerns of painless deliveries is the safety of neonates. This clinical trial study aimed to compare the effects of epidural and spinal anesthesia on the mortality rate of neonates.
Methods: This clinical trial was conducted in Hamadan Hospital in Iran. Ninety women, ages 18 to 45, were randomly assigned to receive epidural or subdural anesthesia. Using a checklist, the following were collected: demographic information, midwifery, hemodynamic status, mothers' pain intensity, and analyses of the baby's umbilical cord blood. The data were analyzed by SPSS version 16 for statistical analysis. Twenty-two of the patients with spinal anesthesia and epidural anesthesia were excluded from the study.
Results: There was no significant difference between the two groups in terms of age, gestational age, parity, and severity of pain before or after anesthesia. The hemodynamic status of the mothers before and during the first postoperative period was in the normal range, except that in the spinal group, a decrease in systolic blood pressure was observed in normal range compared with the epidural anesthesia group. In blood gas analysis, the mean pH, partial pressure of carbon dioxide (PCO2), and bicarbonate (HCO3) did not show significant differences between the two groups (p > 0.05). The only complications were acidosis and epidural anesthesia.
Conclusion: Based on the findings of the present study, both spinal and epidural opioids have no adverse effects on the health of neonates. However, both spinal and epidural opioid are preferred due to fewer changes in the hemodynamic changes in mothers and in umbilical cord blood gas.
INTRODUCTION
Pregnancy is carried out in a variety of ways which include standard vaginal delivery and cesarean section. Natural childbirth is carried out in two ways- with painless and without pain control. The pain of vaginal delivery is one of the hardest pains that women can experience during their life1.
One of the essential methods used to reduce the extent of labor pain in the developed world in recent decades is the use of such local epidural and spinal anesthesia2.
The pain of vaginal delivery varies widely but many women consider the pain to be unbearable. The pain during pregnancy and vaginal delivery is caused by uterus contractions, cervical enlargement, and stretching of the perinea. The visceral and somatic marker fibers are transmitted to the spinal cord along with sympathetic nervous fibers (via the T10-T12 and L1 nerve impulses) then through the uterus (via T12 and L1 nerve impulses); somatic nerve impulses (S2-S4) are transmitted to sacral nerves 2, 3 and 43.
Various factors affect the perception of delivery; these include duration, anatomy of the mother, size of the embryo, use of oxytocin, prenatal mortality, fear, as well as anxiety from childbirth, behavior, and experience of pain and adaptive systems. The lack of proper control of acute pain is associated with destructive pathophysiologic effects. Moreover, mothers show a higher tendency to lean towards natural delivery, along with pain control, over a cesarean section which is a significant operation4.
Inadequate control of labor pain is associated with adverse effects on both the mother and fetus. For example, in the respiratory system, an increase in the respiratory rate resulted from a decrease in uterine and brain blood flow. Lumbar spinal anesthesia is a safe method for the relief of labor pain. Using low amounts of local and narcotic analgesics, lumbar epidural anesthesia is an effective sensory anesthesia in the first stage of delivery (t10-l1) and may be needed in the continuation of labor to block completion4.
One of the challenges of local anesthesia (e.g. spinal or epidural) is their effects on the fetus and its hemodynamic status. Epidural anesthesia causes pain reduction, which is associated with increased breathing rate; changes of hemoglobin in the mother can have a negative effect on neonatal hemoglobin5.
Regional imbalances may result in uterine contraction by the sympathetic nervous system, although it is a useful effect in delivery. If the sympathetic nerve block is extended, the blood flow rate of the umbilicus can also be reduced6. The amount of dissolved oxygen in the fetus falls between 20 to 96 % during labor, and can be considered as a threshold that is associated with fetal distress7. A change occurs in 15 – 24 % of the cases in the fetal heart rate after performing a painless method of delivery8. Given the lack of studies in the field, as well as lack of policy in the country to promote natural childbirth, this clinical trial study herein was aimed at comparing epidural and spinal anesthesia in newborn babies.
METHODS
This study herein was a clinical trial study which was carried out at the Hospital in Hamadan (Iran). The study population consisted of 90 patients who had no prior anesthesia.
The inclusion criteria were: first pregnancy or second pregnancy, in an active phase of labor, more than 37 weeks of gestation, single pregnancy, vertex presentation, lack of any underlying disease, women between 18 – 45 years of age, as well as pregnant women aged 37 to 42 weeks who attended Fatemieh Hospital (Iran) for normal vaginal delivery and were without control candidates. The exclusion criteria were: use of drugs by patient in operation, unwillingness to participate in the study, and lack of literacy.
Prior to the beginning of the study, all participants had reviewed, agreed to, and provided written consent to participate in the trial. Initially, the technique of work to be done for each patient was explained, accounting for the culture and the patient's level of education. Then, the patients were randomly divided into two groups. For all patients, an intravenous line was taken; at the beginning of the study, 500 to 1000 mL sodium chloride 0.9 % were infused.
In the spinal patient group, the patient was seated in a sitting position using a–the needle number of 25 spinal needles (Dr. Japan Co Ltd.) and 2 ml of Sufentanil in the subarachnoid area.
In the epidural group, firstly, an empty needle number of 18 (Ogame Turkiye) was inserted into the epidural apace from the interlayer space (L3 and L4) using a loss of resistance method and without using needle tests. Then, the epidural catheter (No 19), 2-3 cm in space, was inserted. After aspiration and Ensure the catheter is in the epidural space, 12 cc of Bupivacaine (0.125 %) was injected along with 2 cc of Sufentanil (in the form of Bolus injection). If a patient requested again for analgesia, 8-10 cc of Bupivacaine (0.125 %) was injected. The patient was put immediately into the supine position, and vital signs were taken, including blood pressure (systolic and diastolic), heart rate before the beginning of drug administration, heart rate at zero minute and every 5 minutes until 15 minutes, and heart rate every 15 minutes until the birth. The severity of the patient's pain was recorded by the patient according to the Visual Analog Scale (VAS) for pain; the patient was asked to give a degree of pain between 0 to 10 such that a grade of ‘10’ was the maximum pain the patient could experience.
Immediately after the birth and primary care of the umbilical cord, the umbilical cord blood was taken with a syringe soaked in heparin and was sent to the laboratory in standard conditions for analyzing blood gases.
Randomization
For this purpose, we used random blocks of 4. In this way, we used 4 paper sheets on two sheets of letter 1 means spinal and on two sheets of letter 2 means epidural, representing the epidural options. The papers were mixed and placed in a table drawer; each patient was assigned one of the papers randomly and thus assigned to one of the epidural or subdural hematomas. It should be noted that the pages were drawn until all four drawn papers were not selected; they were then returned to the drawer. After the last sheet had been drawn again, the sheets were again returned to the drawer. The above procedure for the next four patients was followed; this sampling method in a row (called consecutive sampling) was done on women who were eligible to enter the study9.
The study design involved measurement of the hemodynamic status of patients. According to the study results1, and using the statistical software Stata to assess sample size in each group, the study sample size consisted of 45 pregnant women with first or second pregnancy, were in an active phase of labor, were past 37 weeks of gestation, had single pregnancy, had vertex presentation, and lacked of any underlying disease. Contraindications for natural childbirth include placenta previa, breech presentation, transverse presentation, fetus weight more than 4.5 kg, history of cesarean section, and underlying diseases (such as cardiac disease, asthma and/or renal disease).
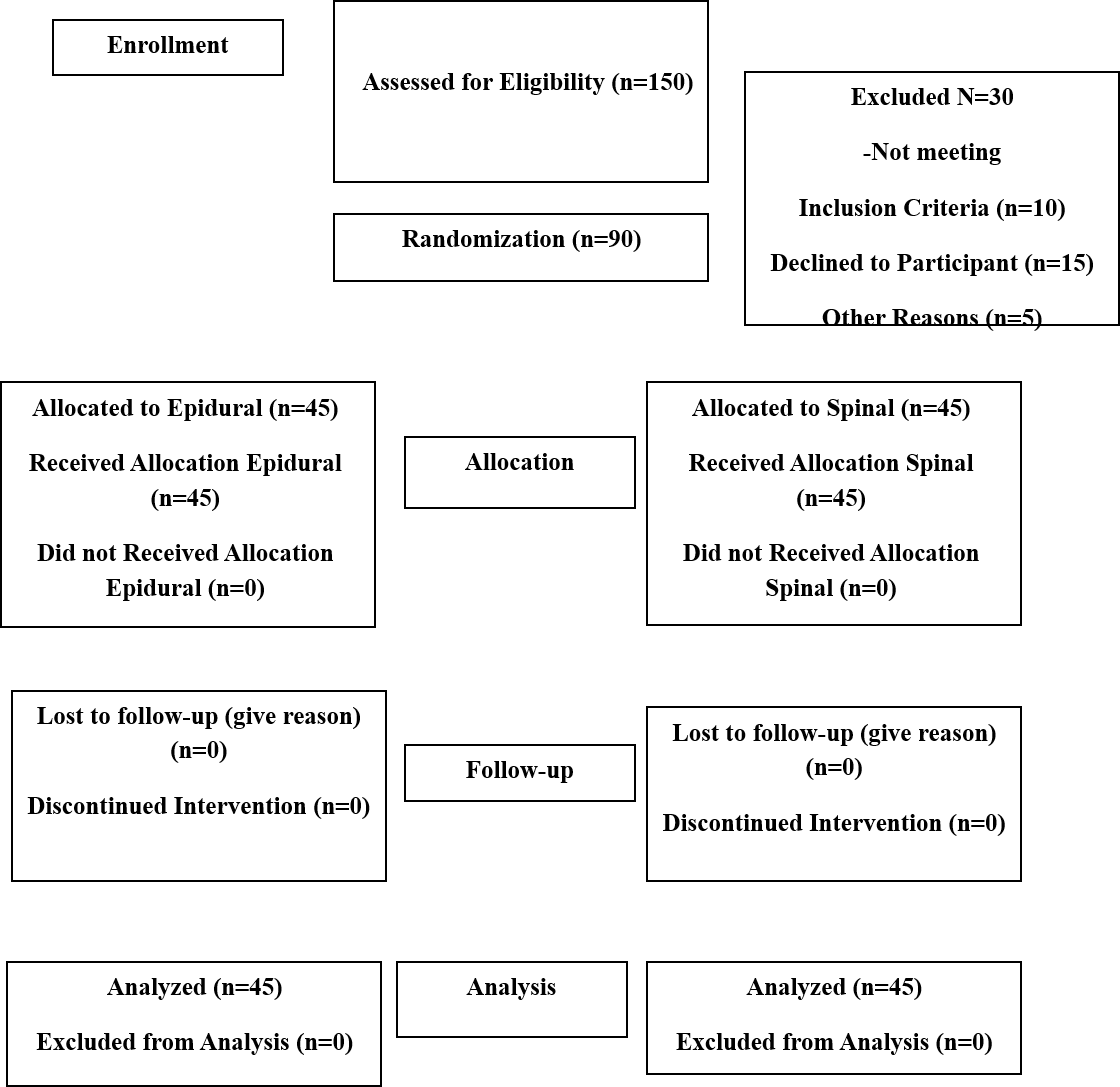
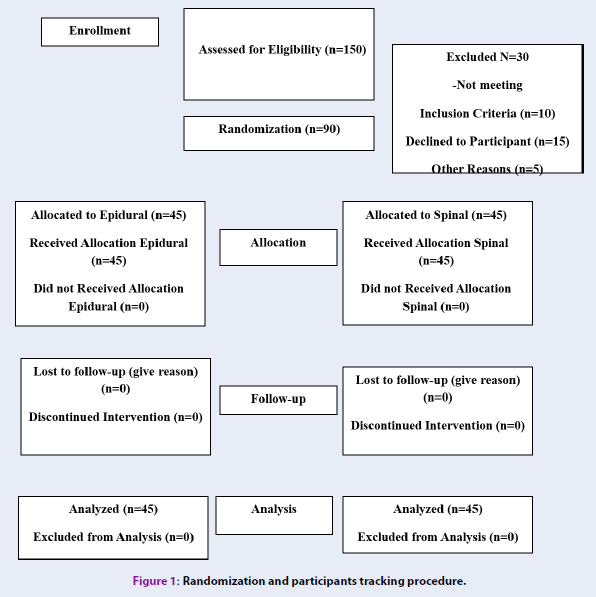
A total number of 90 individuals entered this clinical study (Figure 1). This study was approved by the Committee on Ethics of the Vice-Chancellor of Research and Technology of Hamadan University of Medical Sciences (IR.UMSHA.REC.1397.496).
Data analysis
Descriptive statistics were carried out; mean and standard deviation were recorded for the quantitative variables, and ratios and percentages were recorded for qualitative variables. In order to compare the relevance of qualitative variables to each other, and quantitative variables, chi-square test (Chi) was used. In this study, SPSS version 16 was used for data analysis. The statistical significance level was set as P < 0.05.
Research limitations
Limitations included the number of patients to participate in this study of the magnitude of pain intensity. Pain was based on the patient’s judgment. This study was done in coordination with the University of Medical Sciences. Informed consent was obtained from patients before their participation in the study. Whether the patients were referrals to the treatment services or not, there was no effect on diagnosis or treatment. The study data were collected without the inclusion of names and individual characteristics.
The study was conducted in coordination with the University of Medical Sciences. Patients were taken into the study after informed consent. Whether the person visited the university had not impacted on their diagnosis or therapeutics. The study data were collected without listing patient names and individual specifications; the results were generalized.
RESULTS
In this clinical trial study, 90 pregnant women were nominated for a normal vaginal delivery and without pain control patients were split into 2 respective groups: epidural (2) and spinal anesthesia (2).
Eleven patients (12.2 %) of the epidural and spinal groups were excluded from the epidural group due to conditions (e.g. deceleration of fetal heart rate, no failure to the progress of delivery, etc.); in fact, they were excluded from the study. Therefore, 40 patients in the spinal group and 39 patients in the epidural group were monitored and evaluated (Table 1).
| Childbirth | Epidural (n (%)) | Spinal (n (%)) | p-value |
|---|---|---|---|
| Normal vaginal delivery | 39 (86.7) | 40 (88.9) | 0.748 |
| Cesarean | 6 (13.3) | 5 (11.1) | |
| Total | 45 (100) | 45 (100) |
It is to noteworthy that in the epidural group, 5 patients (due to arrest of dilatation) and 1 patient (due to fetal distress) underwent cesarean section. Also, in the spinal group, 1 patient (due to arrest) and 4 patients (due to fetal distress) had cesarean sections.
The mean and standard deviation of age in the spinal group and in the epidural group were 23.2 ± 5.3 and 22.8 ± 4.3, respectively. Comparing the two groups, the average age (p = 0.919), pregnancy age (p = 0.430), pregnancy number (p = 0.919), and severity of pain before (p = 0.579) and after anesthesia (p = 0.189) were not significantly different (Table 2).
| Variable | Spinal (M±SD) | Epidural (M±SD) | p-value |
|---|---|---|---|
| Age | 23.2 ± 5.3 | 22.8 ± 4.3 | 0.919 |
| Pregnancy age (week) | 39 ± 1.4 | 39.1 ± 2.4 | 0.430 |
| Pregnancy number | 1.2 ± 0.5 | 1.3 ± 0.6 | 0.919 |
| vas (pre - analgesic) | 6.2 ± 12 | 6.3 ± 1.2 | 0.579 |
| vas (post - analgesic) | 2.6 ± 0.8 | 2.6 ± 1.3 | 0.187 |
The results of the study showed that before the operation, hemodynamic variables and all other variables across the two groups were comparable. For the patients of the spinal group, blood pressure reduction following the infusion of anesthesia was found to be significant with subdural hematomas, although the changes were not outside the normal range. At other times, the blood pressure of systolic and diastolic in patients with numbness of spinal anesthesia was less than that of epidural; however, there was no significant difference. In both groups, the fetal heart rate and Apgar of neonates were in the normal range and were comparable (Table 3).
| Variable | Spinal (M ± SD) | Epidural (M ± SD) | p-value |
|---|---|---|---|
| Systolic (pre-analgestic) | 120.3 ± 4.6 | 119.3 ± 7.6 | 0.319 |
| Diastolic (pre-analgestic) | 68.1 ± 9.9 | 66.2 ± 7.4 | 0.243 |
| Systolic (post - analgesic) | 117.6 ± 7.2 | 122.9 ± 10.6 | 0.006 |
| Diastolic (post - analgesic) | 73.2 ± 9.8 | 75 ± 7.9 | 0.716 |
| Systolic (5 minutes later) | 116.3 ± 7.6 | 120.3 ± 10.1 | 0.064 |
| Diastolic (5 minutes later) | 73 ± 9.8 | 73.6 ± 7.7 | 0.767 |
| Systolic (10 minutes later) | 115.2 ± 9.9 | 117.1 ± 10.9 | 0.370 |
| Diastolic (10 minutes later) | 71.4 ± 10.2 | 73.7 ± 11.1 | 0.305 |
| Fetal heart rate (pre-analgestic) | 138.9 ± 4.3 | 136.7 ± 6.4 | 0.121 |
| Fetal heart rate (10 minutes later) | 136.4 ± 12.1 | 136.9 ± 5.2 | 0.356 |
| Apgar (1 minute later) | 8.9 ± 0.5 | 8.9 ± 0.4 | 0.789 |
| Apgar (5 minutes later) | 9.9 ± 0.3 | 9.9 ± 0.2 | 0.697 |
The findings indicated that the average pH in the two groups was not statistically significant (p = 0.313) and that the pH of the groups was in the natural range (7.3). Theoretically, both groups were within the normal range. The mean values of partial pressure of oxygen (PO2) of both groups were in the normal range but were less than that for epidural, with a significant difference in the patients (p = 0.017) (Table 4).
| Variable | Spinal (M ± SD) | Epidural (M ± SD) | p-value |
|---|---|---|---|
| PH | 7.3 ± 0.07 | 7.3 ± 0.08 | 0.313 |
| PCO2 | 40.1 ± 9.7 | 42.1 ± 12.6 | 0.432 |
| HCO3 | 21.6 ± 6.1 | 19.9 ± 4.4 | 0.150 |
| PO2 | 19.1 ± 11.9 | 24.8 ± 16.5 | 0.017 |
| Base Deficit | 3.3 ± 2.6 | 3.4 ± 2.5 | 0.576 |
| Hematocrit | 44.4 ± 8.1 | 43.6 ± 7.7 | 0.666 |
The findings indicated that there was observed acidosis in only 2 patients, both of them were in the epidural group, and which was not statistically significant (p = 0.241) (Table 5, Table 3).
| Condition | Spinal (mg/dl) | Epidural (mg/dl) | p-value |
|---|---|---|---|
| Acidosis | - | 2 (5.1) | 0.241 |
| Normal | 40 (100.0) | 437 (94.8) | |
| Total | 40 (100.0) | 39 (100.0) |
DISCUSSION
This clinical trial was aimed at comparing the effects of epidural anesthesia and spinal anesthesia on the amount of anesthetics and newborn blood gases in a normal delivery method at an educational center.
The results of the present study showed that painless delivery does not adversely affect the neonates so that the average Apgar coefficient between the two groups in the first and fifth minute was approximately 9 and higher. In the analysis of the umbilical cord blood gases, it was found that the average pH in the two groups was not statistically significant, and that the blood pH of the umbilical cord blood was both within the natural range.
The fetal heart rate (FHR) was also normal after the numbness in the normal range, and bradycardia did not occur in neonates. Moreover, there was no effect on the maternal side, and the hemodynamic changes were within the normal range. Both groups of women had a desired state of the condition, and the mean of pain intensity using the VAS scale was approximately 2.5 % after the anesthetic injection at the delivery stage.
In this study, the patients of the 2 groups were studied in terms of parity, age, Apgar score, hemodynamic status of mothers before and after anesthesia, and class. There was found to be no significant differences between the two groups. Therefore, the results of this study cannot be affected by those confounding variables.
The pain of childbirth is one of the hardest pains a woman experiences in her life1. Over the years, it has been trying to relieve the pain by taking measures like inhalation of nitrogen (N2), acupuncture, hydrography, and use of opium. However, these measures were usually not satisfactory at reducing pain. The introduction of spinal analgesia (epidural and spinal anesthesia, or combination of these two methods) has been one of the most dramatic developments in the control of labor pain, which has been accompanied by maternal satisfaction and the sanctity of the embryo and baby10.
Currently, approximately 60 % of women in the United States use painless methods11. After spinal cord anesthesia, the heart rate may undergo changes such as those associated with bradycardia. The amount of FHR changes after spinal anesthesia varies between 15 and 25 %12. FHR was not used for painless delivery. The patient must be able to provide painless drugs in all delivery stages and have no adverse effects on fetus and neonates, which in the present study; There was no painless effect and there was lack of undesirable effects on the fetus.
Different studies have examined the effects of region on childbirth and its consequences. According to outcome analysis, the type of medicine has been reported for different results from different results. In a case study - evidence in 201013, the findings of this study revealed that the rate section, umbilical cord blood gases, Apgar scores, and baby outcome in anesthesia patients confirm the findings of this study.
Moreover, the results of another study14 showed that patients with epidural anesthesia were not abnormal, even in the first half hours after the administration of anesthetia. In another study, a relatively small sample volume of low sample size has been carried out from the epidural — spinal method with significant changes of painless childbirth. It was also observed that after the numbness of significant changes (such as in the heart rate of the embryo), the incidence of bradycardia aligns with the findings of the present study.
Reynolds et al., in a study, found that Epichlorohydrin would reduce the blood pressure of the mother and fever, as well as increase in the second stage of labor and the use of a vacuum for the birth of vaginal delivery. However, the latter duty is negligible in the face of the risk reduction of acidosis in neonates15.
In the present study, there were only 5 % of patients who had acidosis and who did not pose as a serious threat to the neonates. It has been shown if the epidural is not carried out at the right time, it may be accompanied by a cesarean section risk13. In this study, 10 – 13 % in both groups eventually had cesarean sections; of these, there were 83 % in the epidural and 20 % in the spinal group due to arrest dilatation. In fact, the epidural group (17 %) and the spinal group (80 %) experienced fetal distress which led to cesarean section.
In a study published in the Cochran database, the epidural is accompanied by an increase in the second phase of labor and a cesarean section risk16. Considering that the conventional method for low sample size is the epidural or spinal anesthesia, most studies have examined these techniques, although the spinal technique may also be widely used due to neurological sequels 17.
One of the advantages of epidural analgesia is that it reduces the need for systemic drugs that may result in neonatal respiratory depression. On the other hand, pain reduction leads to a decrease in the endogenous opioid secretion. The advantage of epidural injection is the possibility of a sensory block without motor block, and minimum hemodynamic complications, and reducing catecholamines. In the present study, hemodynamic changes in the epidural group were less than those for the spinal group.
On the other hand, people are also considering health and treatment policies. These are based on the fact that elective cesarean can be reduced and one of the women worries to have normal vaginal delivery. However, the women are associated with it since it is has been determined that this method is accompanied by pain relief and lack of serious complications.
CONCLUSIONS
According to the findings of this study, both the spinal and epidural methods have adverse effects on infant health. However, given that the epidural induces fewer changes to hemodynamics and maternal umbilical cord blood gas low sample size.
ABBREVIATION
FHR: Fetus Heart Rate
VAS: Visual Analog Scale
AOUTHORS' CONTRIBUTIONS
All authors contributed equally in the study design, interpretation of the data and writing of the final manuscript.
COMPETING INTERESTS
The author(s) declare that they have no competing interests.
This study was supported by Hamadan University of Medical Sciences.
ACKNOWLEDGMENTS
We thank the manager of Fatemieh hospital and also participants to participate in this study.
References
-
Melzack
R.,
The myth of painless childbirth (the John J Bonica lecture). Pain.
1984;
19
:
321-337
.
View Article PubMed Google Scholar -
Konefal
H.,
Jaskot
B.,
Czeszynska
MB.,
Pethidine for labor analgesia; monitoring of newborn heart rate, blood pressure and oxygen saturation during the first 24 hours after the delivery. Epub 2012/06/20. Petydyna w analgezji porodu; monitorowanie czynnosci serca, cisnienia tetniczego i saturacji w ciagu pierwszych 24 godzin zycia noworodka. pol. Ginekol Pol.
2012;
83
(5)
:
357-362
.
PubMed Google Scholar -
Miller
RD.,
Eriksson
LL.,
Fliesher
LA.,
Winer-Kronish JP. Miller's anesthesia. 6 ed. New York: McGraw-Hill.
2005
.
-
Rolfseng
OK.,
Skogvoll
E.,
Borchgrevink
PC.,
Epidural bupivacaine with sufentanyl or fentanyl during labour, a randomized double blind study. Eurk J Anesthesiol.
2002;
19
(11)
:
812-818
.
View Article PubMed Google Scholar -
Scherer
R.,
Holzgreve
W.,
Influence of epidural analgesia on fetal and neonatal well-being. Eur J Obstet Gynecol Reprod Biol.
1995;
59
:
17-29
.
View Article PubMed Google Scholar -
Eberle
RL.,
Norris
MC.,
Eberle
AM.,
Naulty
JS.,
VA. Arkoosh,
The effect of maternal position on fetal heart rate during epidural or intrathecal labor analgesia. Am J Obstet Gynecol .
1998;
179
:
150-155
.
View Article PubMed Google Scholar -
Goffinet
F.,
Langer
B.,
Carbonne
B.,
Multicenter study on the clinical value of fetal pulse oximetry. I. Methodologic evaluation.The French Study Group on Fetal Pulse Oximetry. Am J Obstet Gynecol.
1997;
177
:
1238-1246
.
View Article PubMed Google Scholar -
Palmer
CM.,
Maciulla
JE.,
Cork
RC.,
Nogami
WM.,
Gossler
K.,
Alves
D.,
The incidence of fetal heart rate changes after intrathecal fentanyl labor analgesia. Anesth Analg.
1999;
88
:
577-581
.
View Article PubMed Google Scholar -
Caliskan
E.,
D. Ozdamar,
Doger
E.,
Cakiroglu
Y.,
A
Kus,
Corakci
A.,
Prospective case control comparison of fetal intrapartum oxygen saturations during epidural analgesia. Int J Obstet Anesth.
2010 ;
19
(1)
:
77-81
.
View Article PubMed Google Scholar -
Hawkins
JL.,
Gibbs
CP.,
Orleans
M.,
Obstetric anesthesia work force survey, 1981 versus 1992. Anesthesiology .
1997;
87
:
135-143
.
View Article PubMed Google Scholar -
Grant
EN.,
Tao
W.,
Craig
M.,
McIntire
D.,
Leveno
K.,
Neuraxial analgesia effects on labour progression: facts, fallacies, uncertainties and the future. BJOG : an international journal of obstetrics and gynaecology.
2015 ;
122
(3)
:
288-293
.
View Article PubMed Google Scholar -
Palmer
CM.,
Maciulla
JE.,
Cork
RC.,
Nogami
WM.,
Gossler
K.,
Alves
D.,
The incidence of fetal heart rate changes after intrathecal fentanyl labor analgesia. Anesth Analg.
1999;
88
:
577-581
.
View Article PubMed Google Scholar -
Zhang
J.,
Landy
H.,
Branch
DW.,
Burkman
R.,
Haberman
S.,
Gregory
KD.,
Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstetrics and Gynecology.
2010;
116
(6)
:
1281-1287
.
View Article PubMed Google Scholar -
Caracostea
G.,
Stamatian
F.,
Lerintiu
M.,
Herghea
D.,
The influence of maternal epidural analgesia upon intrapartum fetal oxygenation. J Matern Fetal Neonatal Med.
2007 ;
20
(2)
:
161-165
.
View Article PubMed Google Scholar -
Reynolds
F.,
Sharma
SK.,
Seed
PT.,
Analgesia in labour and fetal acid-base balance: a meta-analysis comparing epidural with systemic opioid analgesia. BJOG : an international journal of obstetrics and gynaecology.
2002;
109
(12)
:
1344-1353
.
View Article PubMed Google Scholar -
Anim-Somuah
M.,
Smyth
R.,
Jones
L.,
Epidural versus non-epidural or no analgesia in labour (Review). The Cochrane Database of Systematic Reviews.
2011;
12 CD000331
.
View Article PubMed Google Scholar -
Hattler
J.,
Klimek
M.,
Rossaint
R.,
Heesen
M.,
The Effect of Combined Spinal-Epidural Versus Epidural Analgesia in Laboring Women on Nonreassuring Fetal Heart Rate Tracings: Systematic Review and Meta-analysis. 2016 ;
123
(4)
:
955-964
.
View Article PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 7 No 3 (2020)
Page No.: 3686-3692
Published on: 2020-03-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 4435 times
- PDF downloaded - 1103 times
- XML downloaded - 0 times
 Biomedpress
Biomedpress