Abstract
Introduction: This study aimed to evaluate the rate of preterm birth and low birth weight in neonates having postnatal respiratory failure.
Methods: A cross-sectional design was used in the study. There were 139 neonates with postnatal respiratory failure and 278 neonates without respiratory failure included in the study. Data on comorbidities, gestational age, and mechanical ventilation status were collected.
Results: Among neonates with respiratory failure, the rate of preterm birth (< 37 weeks) was 70.5%. The average gestational age and weight of the respiratory failure group were significantly lower compared to the control group (p < 0.001). Asphyxia, patent ductus arteriosus, and hyaline membrane were the most common causes of respiratory failure. The rate of neonates having less than 37 gestational weeks and requiring mechanical ventilation as treatment for respiratory failure was 73.5%, in which the proportion of neonates born before 32 gestational weeks was 47.1% (p < 0.001).
Conclusion: The rates of preterm birth and low birth weight among infants with respiratory failure in a tertiary hospital in Vietnam were significantly high. Causes of preterm birth and low birth weight were preventable and treatable if having appropriate care and treatment plan.
INTRODUCTION
Respiratory failure is a common phenomenon in neonates and a main cause of neonatal treatment in intensive care units. A previous report indicated that one-third of neonates with respiratory failure who were hospitalized were preterm infants1. The mortality rate of preterm birth is high in Vietnam. Data of the World Health Organization (WHO) reported that 18% of premature babies died in Vietnam in 20122. Hyaline membrane disease, meconium aspiration syndrome, pneumonia, pulmonary hemorrhage, and congenital heart defects are the leading causes of respiratory failure2, 3. Previous reports in the literature have shown that gestational age and birth weight have bidirectional associations with neonatal respiratory failure4, 5, 6, 7.
Although preterm birth and low birth weight in neonates with postnatal respiratory failure are thoroughly investigated in the literature, limited evidence has been found in Vietnam. This study aimed to measure the rate of preterm birth and low birth weight in neonates with postnatal respiratory failure in Bach Mai Hospital, a tertiary hospital in Vietnam. This information will help clinicians to develop care and treatment protocols, support resuscitations, and have appropriate post-natal care after birth in order to limit complications of postnatal respiratory failure.
METHODS
Study design and participants
A cross-sectional study was conducted at the neonatal Intensive Care Unit (ICU) at the Department of Pediatrics, Bach Mai Hospital, from 1/2015 to 12/2018. A total of 417 neonates born in the Department of Obstetrics, Bach Mai Hospital, and then admitted to the ICU of the Pediatrics Department (Bach Mai Hospital, between 1/2015 and 12/2018) were included in the study. They were divided into two groups: 1) the case group consisting of 139 neonates having postnatal respiratory failure; and 2) the control group consisting of 278 neonates hospitalized for other causes instead of respiratory failure.
Acute respiratory failure is defined as lung dysfunction which causes failure in balancing oxygen and carbon dioxide, leading to uncontrolled PaO2 (partial pressure of oxygen), PaCO2 (partial pressure of carbon dioxide), and pH in the lung8. Infants with the following clinical symptoms could be diagnosed with respiratory failure: 1) Rapid breathing with > 60 breaths/min or slow breathing with < 40 breaths/min; 2) Chest wall retractions or paradoxical movement of the chest wall; 3) Nasal flaring; 4) Long breathing or apnea; 5) Cyanosis when breathing; and 6) Apgar score at the 1st and 5th minute after being born (total score: ≤ 3: severe asphyxia, 4–6 points: moderate asphyxia, ≥ 7: normal). Moreover, results of blood gas and pulmonary X-ray could be used as supplements8, including: 1) Pa02 < 60mmHg, and/or PaCO2 > 50mmHg and pH < 7.1–7.2; 2) Badly enlarged bilateral lungs, ground-glass opacity nodules, or stagnant air in a large bronchus, and even white lungs occurring if the disease was severe9.
In this study, all newborns with respiratory failure were diagnosed by pediatricians with at least five years of experience in the newborn care unit at the Obstetrics and Gynecology Department of Bach Mai hospital. When they were admitted to the neonate ICU of the Department of Pediatrics, all of them had undergone cardiac ultrasound. They were also scanned for cardiac conditions during the treatment period by pediatric radiologists.
Data sources and measurements
Premature infants were defined as neonates who had gestational ages less than 37 weeks or less than 259 days. According to gestational age, infants could be divided into four groups: 1) Extremely preterm (24 to < 28 weeks); 2) Very preterm (28 to < 32 weeks); 3) Preterm infants (32 to < 37 weeks); and Full-term infants (37 – 42 weeks).
Infants with a birth weight below 2500 g were classified as low birth weight3. They could be categorized into: 1) Low weight (1,500 g to < 2,500 g); 2) Very low weight (1,000 g to < 1,500 g); and 3) Extremely low weight (< 1,000g).
Data about causes of gestational age and low birth weight, and whether infants received mechanical ventilation or not were also collected.
Statistical Analysis
We compared gestational age and birth weight between two study groups with and without respiratory distress. T-test was used to compare the means of birth weight and gestational age. Chi-squared and Fisher’s exact tests were used to detect the differences between both groups. Odds ratio was calculated to examine the association between low birth weight and respiratory failure. Two-sided p-value < 0.05 was considered statistically significant.
Ethical approval
The Institutional Review Board of the Bach Mai Hospital approved the protocol of this study (Code 3534/QD-BM).
RESULTS
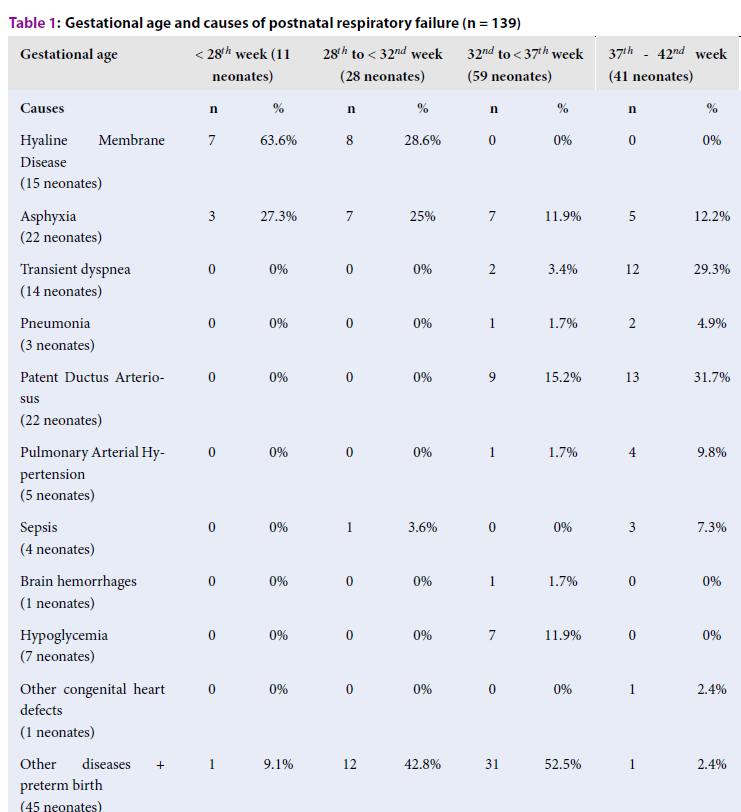
The mean gestational age of the case group was 34 weeks, which was lower than that of the control group (mean = 38 weeks) (p < 0.001). The mean weight in the case group was 2,057 g, which was lower than the control group (mean = 2,893 g) (p < 0.001). Hyaline membrane disease occurred on neonates with less than 32 weeks of gestational age. Asphyxia occurred in all ages, transient dyspnea predominantly occurred in full-term infants (37 – 42 weeks), and cardiovascular disease occurred in gestational age of greater than 32 weeks.
| Gestational age | < 28th week (11 neonates) | 28th to < 32nd week (28 neonates) | 32nd to < 37th week (59 neonates) | 37th - 42nd week (41 neonates) | ||||
| Causes | n | % | n | % | n | % | n | % |
| Hyaline Membrane Disease (15 neonates) | 7 | 63.6% | 8 | 28.6% | 0 | 0% | 0 | 0% |
| Asphyxia (22 neonates) | 3 | 27.3% | 7 | 25% | 7 | 11.9% | 5 | 12.2% |
| Transient dyspnea (14 neonates) | 0 | 0% | 0 | 0% | 2 | 3.4% | 12 | 29.3% |
| Pneumonia (3 neonates) | 0 | 0% | 0 | 0% | 1 | 1.7% | 2 | 4.9% |
| Patent Ductus Arteriosus (22 neonates) | 0 | 0% | 0 | 0% | 9 | 15.2% | 13 | 31.7% |
| Pulmonary Arterial Hypertension (5 neonates) | 0 | 0% | 0 | 0% | 1 | 1.7% | 4 | 9.8% |
| Sepsis (4 neonates) | 0 | 0% | 1 | 3.6% | 0 | 0% | 3 | 7.3% |
| Brain hemorrhages (1 neonates) | 0 | 0% | 0 | 0% | 1 | 1.7% | 0 | 0% |
| Hypoglycemia (7 neonates) | 0 | 0% | 0 | 0% | 7 | 11.9% | 0 | 0% |
| Other congenital heart defects (1 neonates) | 0 | 0% | 0 | 0% | 0 | 0% | 1 | 2.4% |
| Other diseases + preterm birth (45 neonates) | 1 | 9.1% | 12 | 42.8% | 31 | 52.5% | 1 | 2.4% |
| Gestational age | Gestational age (weeks) | Average gestational | |||
| Child patient | < 28 | 28 to < 32 | 32 to < 37 | 37 - 42 | Age (X ± SD) |
| Respiratory failure (139 neonates) | 11 | 28 | 59 | 41 | 34.02 ± 4.27 |
| 7.9% | 20.1% | 42.5% | 29.5% | ||
| Non respiratory failure (278 neonates) | 0 | 1 | 66 | 211 | 38.13 ± 2.09 |
| 0% | 0.4% | 23.7% | 75.9% | ||
| p - value | < 0.001 | < 0.001 | |||
| Gestational age | Mechanical ventilation (68 neonates) | Non mechanical ventilation(71 neonates) | ||
| n | % | n | % | |
| < 28th week | 11 | 16.2 | 0 | 0 |
| 28th to < 32nd week | 21 | 30.9 | 7 | 9.9 |
| 32th to < 37th week | 18 | 26.5 | 41 | 57.7 |
| 37nd – 42nd week | 18 | 26.5 | 23 | 32.4 |
| p - value | < 0.001 | |||
| Weight | Birth weight (g) | Average weight (X ± SD) | ||||
| Group | < 1,000 | 1,000 to < 1,500 | 1,500 to < 2,500 | 2,500 to 3,500 | > 3,500 | |
| Respiratory failure (139 neonates) | 18 | 24 | 49 | 39 | 9 | 2,056.9 ± 939.3 |
| 13% | 17.3% | 35.2% | 28% | 6.5% | ||
| Non respiratory failure (278 neonates) | 0 | 3 | 70 | 165 | 40 | 2,893.3 ± 608.6 |
| 0.0% | 1.1% | 25.2% | 59.3% | 14.4% | ||
| p - value | < 0.001 | < 0.001 | ||||
| Group | Respiratory failure(139 neonates) | Non respiratory failure(278 neonates) | p | OR(95%CI) | ||
| Weight | n | % | n | % | ||
| < 2,500 g (164 neonates) | 91 | 65.5 | 73 | 26.3 | < 0.01 | 5.324(3.429 - 8.267) |
| ≥ 2,500g (253 neonates) | 48 | 34.5 | 205 | 73.7 | ||
For neonates with respiratory failure, the rate of preterm infants accounted for 70.5%, of which 42.5% were born at 32 – 37 weeks of gestation. Preterm birth was associated with postnatal respiratory failure (p < 0.001).
The percentage of neonates with less than 37 weeks of gestation requiring mechanical ventilation for respiratory failure was 73.5%, of which neonates with less than 32 weeks of gestation accounted for 47.1%. Preterm birth was associated with postnatal respiratory failure requiring mechanical ventilation (p < 0.001).
The neonatal group having birth weight less than 2,500 g accounted for 65.5% in the respiratory failure group. Low birth weight was associated with a higher risk of postnatal respiratory failure (p < 0.001). The mean birth weight of the respiratory failure group was 2,056.9 ± 939.3 g, which was significantly lower than that of the control group (2,893.3 ± 608.6 g) (p < 0.001).
Of the 139 neonates with respiratory failure, 65.5% had low birth weight (< 2,500 g). Low birth weight was associated with postnatal respiratory failure (p < 0.001). The risk of respiratory failure in low birth weight infants (< 2,500 g) was 5.324 (OR = 5.324, 95% CI: 3.429 – 8.267) times higher than infants with normal birth weight.
DISCUSSION
Our study echoed results from the existing literature, confirming the associations between low birth weight, preterm birth and respiratory failure among neonates. In this study, we found a significant high rate of the above health problems in infants with respiratory failure condition. Our study suggested several clinical implications for designing appropriate management for infants with low birth weight and preterm birth in the context of a tertiary hospital in Vietnam.
In the current study, the rate of preterm birth in infants with respiratory failure was 70.5%, which was significantly higher than that in the non-respiratory failure group. This rate in our study was higher than that of a previous study in Vietnam, which reported that only one-third of premature infants were admitted to the ICU due to respiratory failure1. According to Reuter et al. (2014), respiratory failure might account for up to 7% of full-term infants; among those admitted to the neonate ICU, the rate of respiratory failure was 15% in full-term infants and 29% in preterm infants10. Moreover, Reuter et al. found that neonates with less than 34 weeks of gestational age had a higher rate of respiratory failure10. Our results might be higher due to the fact that our patients were immediately admitted to the ICU after being born at the Department of Obstetrics of Bach Mai Hospital.
Low birth weight causes many postpartum diseases, especially respiratory failure. According to our results, the proportion of neonates weighing less than 2,500 g and suffering from respiratory failure was 65.5%, which was much higher than those without respiratory failure. Liu et al. conducted a study among 205 preterm infants with respiratory failure and also found similar results11. Thus, low birth weight was a risk factor in causing respiratory failure among preterm infants. This risk is able to be controlled when pregnancy and maternal disease were managed strictly.
Of note, our premature infants had higher rates of hyaline membrane disease, asphyxia, and hypoglycemia than those of full-term infants. Our results were similar to those from study by Donn et al. (2006), which showed that hyaline membrane disease occurred predominantly in neonates < 32 weeks3, 12. Anne Greenough et al. found that the rate of hyaline membrane disease was 50% among those with less than 30 weeks of gestational age and only 2% among infants with the gestation age from 35 to 36 weeks12. Jonathan et al. indicated that the rate of pulmonary arterial hypertension in neonates accounted for 5% — 10% of all congenital heart defect cases. In addition, there were about 80% of neonates with acute respiratory failure having pulmonary arterial hypertension; approximately 70% of those with less than 30 weeks of gestation age had patent ductus arteriosus13.
The results of our study herein also showed that the rate of preterm infants requiring mechanical ventilation was 73.5% in the case group, which was higher than that of the control group (67.6%). Among infants with respiratory failure who had gestation age of less than 32 weeks, the rate of infants receiving mechanical ventilation was significantly higher than the rate of infants not requiring non-mechanical ventilation. Thus, it is necessary to manage pregnancy, maternal disease, and monitor risk factors of preterm birth. Also, there is a need for a collaborating mechanism between the Department of Obstetrics and Department of Pediatrics in neonatal resuscitation and care immediately after birth.
This study had some limitations. The study design limits the ability to conclude a causal relationship between preterm birth, low birth weight, respiratory failure, and their consequences. Also, only information on gestational age, birth weight, causes of respiratory failure, and whether or not the outcome was fatal were collected. Other factors, such as potential risks during pregnancy or track disease progression., were not considered. Besides, our study results are not representative because this study was conducted at only one tertiary hospital with small sample size. Therefore, it is not possible to extrapolate results for all premature, low birth weight infants with respiratory distress in Vietnam.
CONCLUSION
The rates of preterm birth and low birth weight among infants with respiratory failure in a tertiary hospital in Vietnam were significantly high. Causes of preterm birth and low birth weight are preventable and treatable if having an appropriate care and treatment plan.
Abbreviations
ICU: Intensive Care Unit
PaCO2: Partial pressure of carbon dioxide
PaO2: Partial pressure of oxygen
WHO: World Health Organization
Acknowledgments
The authors are thankful to Department of Obstetrics and the ICU of the Pediatrics Department (Bach Mai Hospital) for providing the administrative support to do this study.
Author’s contributions
Nguyen Thanh Nam: Conceptualization, Formal analysis, Methodology, Visualization, Writing — original draft, Writing — review & editing. Pham Van Dem: Conceptualization, Investigation, Methodology, Project administration, Validation, Visualization, Writing — original draft, Writing — review & editing. Ngo Thi Tam: Formal analysis, Software, Writing — original draft, Writing — review & editing. Nguyen Tien Dung: Conceptualization, Supervision, Validation, Visualization, Writing — original draft, Writing — review & editing. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was conducted in accordance with the amended Declaration of Helsinki. The Institutional Review Board of the Bach Mai Hospital approved the study, and all participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
Thuong TC. Disease and Mortality of infants at Neonatal Department of Children's 1 Hospital. Journal of Practiccal Medicine.
2014;
708
(3)
:
27-31
.
-
The UN Inter-agency Group for Child Mortality Estimation Mortality rate, infant (per 1,000 live births), The World Bank, acessed date 25/5/2020, at website https://data.worldbank.org/indicator/SP.DYN.IMRT.IN.. 2018
.
-
Bonita F. Stanton and Richard E. Behrman, Overview of Pediatrics, Robert M. Kliegman Nelson Text Book of Pediatrics, 20 th Edition, 2016. Elsevier, Philadelphia, 20-39 .
Google Scholar -
Wen YH, Yang HI, Chou HC, Chen CY, Hsieh WS, Tsou KI, et al. Association of Maternal Preeclampsia with Neonatal Respiratory Distress Syndrome in Very-Low-Birth-Weight Infants. Scientific Reports.
2019;
9
(1)
:
13212
.
View Article PubMed Google Scholar -
Glass HC, Costarino AT, Stayer SA, Brett C, Cladis F, Davis PJ. Outcomes for extremely premature infants. Anesthesia and analgesia.
2015;
120
(6)
:
1337
.
View Article PubMed Google Scholar -
Morley CJ, Davis PG, Doyle LW, Brion LP, Hascoet JM, Carlin JB. Nasal CPAP or intubation at birth for very preterm infants. New England Journal of Medicine.
2008;
358
(7)
:
700-708
.
View Article PubMed Google Scholar -
Finer N, Carlo W, Walsh M. SUPPORT Study Group of the Eunice Kennedy Shriver NICHD Neonatal Research American Board of Pediatrics Neonatal-Perinatal Content Specifications• Plan the ventilatory therapy for infants with respiratory failure of different etiologies.• Know the indications for and techniques of positive pressure ventilation (PPV).• Know the effects and risks of PPV. Network. Early CPAP versus surfactant in extremely preterm infants. The New England journal of medicine.
2010;
362
(21)
:
1970-1979
.
View Article PubMed Google Scholar -
Hoang Thi Duy Huong, Lung disease and respiratory distress of infants, Nguyen Cong Khanh ed, Text book of Pediatrics. Medical Publishing house, Hanoi, 2016. 232-246 .
Google Scholar -
Nguyen Tien Dung. Respiratory Disease in Neonatal Text Book, Medical Publishing house, Hanoi, 2018. 48-60 .
Google Scholar -
Reuter S, Moser CBM. Respiratory Distress in the Newborn. Pediatrics in Review.
2014;
35
(10)
:
417-429
.
View Article PubMed Google Scholar -
Liu JYN, Liu Y, et al. High-risk Factors of Respiratory Distress Syndrome in Term Neonates: A Retrospective Case-control Study. Balkan Med J.
2014;
31
:
64-68
.
View Article PubMed Google Scholar -
GAaM
A.D.,
Ulmonary disease of the newborn-Part 1: Physiology, Rennie and Roberton's Janet M Rennie. Textbook of Neonatology.
2012;
5
:
448-467
.
-
Jonathan L, Slaughter CLC, Jennifer L. Notestine et al. Early prediction of spontaneous Patent Ductus Arteriosus (PDA) closure and PDA-associated outcomes: a prospective cohort investigation. BMC pediatrics.
2019
.
View Article PubMed Google Scholar
Comments
Downloads
Article Details
Volume & Issue : Vol 7 No 9 (2020)
Page No.: 4010-4015
Published on: 2020-09-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 4254 times
- Download PDF downloaded - 1157 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress


